In summary:
Aortic aneurysm is a widening (ballooning) of the aorta, the body’s main artery. It may occur in the abdomen (AAA) or chest (TAA). Many aneurysms cause no symptoms and are found on health screening or unrelated scans, but the key risk is enlargement and rupture. Seek urgent attention for sudden severe chest, back, or abdominal pain, especially if you have a known aneurysm. Diagnosis is usually with ultrasound or CT angiography. Management depends on symptoms, size, and growth rate. Treatment ranges from surveillance and risk-factor control to endovascular stent grafting (EVAR/TEVAR) or open surgery when indicated.
What Is an Aortic Aneurysm?
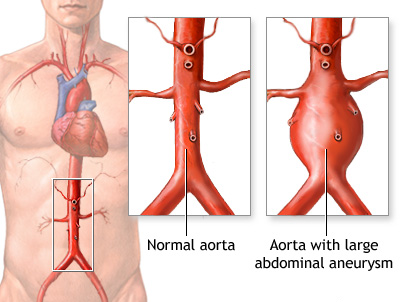
An aortic aneurysm is a serious vascular condition involving the ballooning or bulging of the aorta- the body’s arterial highway that carries oxygen-rich blood from the heart to the rest of the body. These aneurysms usually develop in the abdomen (abdominal aortic aneurysm or AAA) but may also occur in the chest (thoracic aortic aneurysm or TAA) located in the chest.
Picture your aorta like a garden hose running from your heart through your chest and tummy, delivering blood everywhere. If a section weakens, it gradually thins and balloons out- that’s what an aneurysm is. Over time, that weak spot can further enlarge and thin, raising the risk of rupture. Because the aorta plays a vital role in circulation, any weakening in its wall can have life-threatening consequences.
How common are Abdominal Aortic Aneurysms (AAA) ?
Abdominal aortic aneurysms aren’t common in the general population, but they’re not rare either. Globally, about 1% of people aged 30–79 are living with an AAA, with men affected far more often than women (approximately 3-4 times more common in men).
In Asia including Singapore, the overall prevalence sits around ~1.3% but climbs to roughly 2.5–4% in higher-risk groups (typically older men above 60 with cardiovascular risk factors or a smoking history).
Why do Aneurysms form?
In many people, it’s simply due to “wear and tear” of the body mixed with a few nudges from risk factors.
As we age, the aortic wall naturally stiffens and weakens. Smoking is the single biggest culprit, as it directly damages the vessel lining. High blood pressure and atherosclerosis add constant strain and inflammation, encourage a weak spot to balloon over time.
Some of us are also born with a thinner safety margin because of family history or genetic conditions that affect connective tissue in the arteries, and men are affected more often than women.
How do we test for Abdominal Aortic Aneurysms (AAA)?
- Ultrasound of the abdomen (screening): quick, painless, radiation-free.
- CT/MRI scan: used when we need more detail, and for surgical planning.
If you’re male aged 65–75 and have ever smoked, most international guidelines recommend a one-off ultrasound to check your abdominal aorta.
Symptoms and Warning Signs- the “Silent Killer”
Most aortic aneurysms cause no symptoms until they are large or close to rupturing, hence the “silent killer” moniker. Aneurysms often grow quietly for years. Doctors frequently find an abdominal aortic aneurysm during an X-ray, ultrasound, or CT that was ordered for something else, or during a routine check.
Should they eventually become symptomatic, their symptoms depend on where the aneurysm sits- whether in the abdomen or chest.

Abdominal Aortic Aneurysm (AAA) symptoms
An abdominal aortic aneurysm is located in your tummy, usually below the kidneys, where the wall has become weak and stretched.
Most people feel nothing at all. When symptoms do appear, they tend to be gradual and a bit vague, which is why AAAs are often missed until a scan spots them.
What people sometimes notice
- Deep, steady abdominal pain. This usually sits in the centre of the tummy and can drift to the side or groin. It often feels like a persistent ache rather than sharp, stabbing pain.
- Lower back pain. Dull, nagging discomfort in the lower back is common. It may come and go or linger for weeks. Because back pain is so common, this is easy to dismiss as unless an aneurysm scan is done.
- A visible or palpable pulse near the belly button. Some people notice a rhythmic thumping when lying flat. This is more likely if the aneurysm is very large or if you are slim.
Thoracic aortic aneurysm symptoms
A thoracic aortic aneurysm is located in the chest portion of the aorta, near the heart and lungs, where it can press on nearby nerves and airways.
Thoracic aneurysms often cause no symptoms until they are larger, but when they do, it is usually because the bulge is pressing on surrounding structures.
What people sometimes notice
- Deep chest or upper back pain. This can sit behind the breastbone or between the shoulder blades and may feel heavy or pressure-like.
- Hoarseness or a persistent cough. The enlarged aorta can irritate the voice nerve or airway.
- Breathlessness on exertion. Very large aneurysms can press on the lungs or affect how the heart valves work.
- Difficulty swallowing. Less common, but pressure on the oesophagus can make swallowing uncomfortable.
Red flag warning signs and symptoms
Call for an ambulance immediately if any of the following occur. In Singapore,
dial 995.
- Sudden, severe abdominal or back pain, especially if it is unlike your usual ache. This is sometimes described as tearing or ripping in nature.
- Feeling faint, sweaty, or unwell at the same time. Other signs of shock include cold, clammy skin, confusion, or extreme weakness.
These symptoms can indicate an impending or actual rupture and need urgent hospital care. Do not drive yourself. If you have a known aneurysm and develop these symptoms, treat it as an emergency without delay.
Need an expert vascular opinion for your Aneurysm?
Book an appointment with Dr. Darryl Lim today and get a personalized treatment plan.

Treatment and Management Options
Treatment depends on the aneurysm’s size, growth rate, and your overall risk profile.
Conservative Management (“Watch and Wait”)
If an aneurysm is small and the short-term risk is low, we may monitor it closely rather than treat it straight away. The goal is to reduce stress on the aortic wall and slow any further enlargement.
That starts with tackling the risk factors you can control, with smoking cessation and good blood pressure control being the two biggest priorities. In some cases, medications to lower blood pressure and cholesterol are started as well. With these measures in place, the risk of the aneurysm progressing can be reduced, alongside regular follow-up scans to monitor for any change over time.
When Aneurysm Repair is recommended
No single number tells the whole story. Vascular surgeons generally look at five things together: size, shape, how quickly it is growing, whether you have symptoms, and your overall health. The aim is to balance the risk of surgery against the risk of leaving the aneurysm alone.
Typical size and growth thresholds
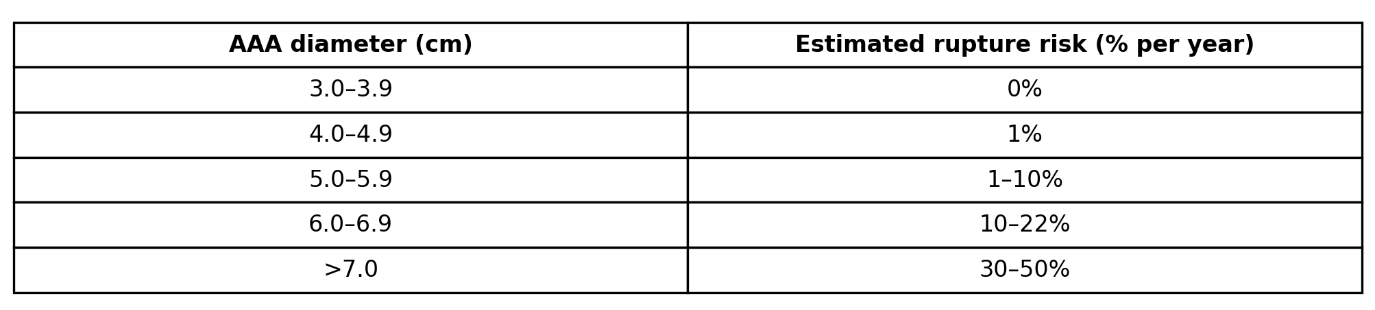
For size, many centres offer repair once an abdominal aortic aneurysm measures about 5.5 cm in men and about 5.0 cm in women. Growth speed also matters: a jump of around 0.5 cm in six months or about 1.0 cm in a year will often bring treatment forward.
Shape matters: fusiform versus saccular
Anatomy also counts- not all aneurysms have the same shape.

Fusiform aneurysm: the aorta widens in a smooth, spindle-like way along a segment. Many AAAs are fusiform and are often suitable for standard surveillance (if size does not meet criteria) and, when needed, for EVAR or open repair.
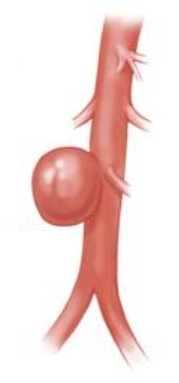
Saccular aneurysm: look more like a pouch on one side of the vessel. Because stress is concentrated, they can behave less predictably and may be repaired at smaller diameters, especially if symptoms are present or the wall looks irregular on CT.
How Vascular Surgeons weigh the decision for surgery
Finally, your overall health and goals are part of the decision. Heart, lung and kidney fitness, previous abdominal surgery, frailty, and how well you are likely to tolerate anaesthesia are weighed against the risk that the aneurysm will rupture in the coming years.
If the risk of rupture is higher than the risk of repair, treatment is usually recommended. Conversely if the aneurysm is small and slow-growing, and your health makes surgery particularly risky, careful surveillance may be safer for now. Your surgeon will explain these trade-offs and help you choose a plan that fits your health and priorities.
Should surgery be recommended, the two primary procedures are Endovascular Aneurysm Repair (EVAR) and Open Surgical Repair.
Endovascular Aneurysm Repair (EVAR)
EVAR is a minimally invasive treatment option which involves inserting a stent graft through small groin incisions and guiding it into position using X-ray imaging. The stent creates a new inner channel for blood, taking pressure off the aneurysm wall.
Compared to open surgery, EVAR offers faster recovery, less pain, and shorter hospital stays, making it the preferred approach for many patients. The caveat is that the aneurysm anatomy must be suitable- the stent needs a good landing zone above and below the aneurysm to seal well.

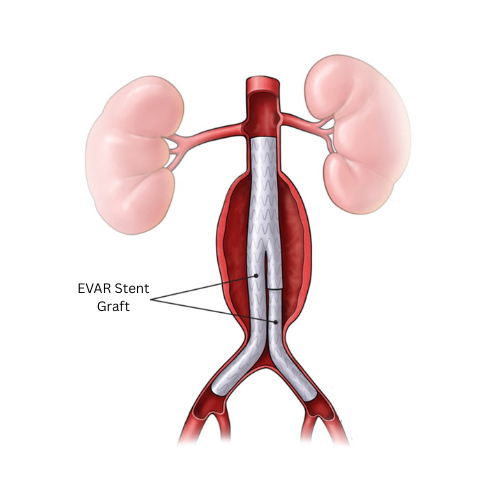
What to expect– In straightforward cases, EVAR is a generally quick procedure with small cuts at the groin. People are usually sitting up the same day and walking a day after surgery. Many get discharged within a couple of days and return to regular daily activities within a week or two.
Lifelong imaging follow-up is important to check graft position and for any endoleaks, which are when a little blood tracks around the graft. Most endoleaks are minor and simply monitored; a few need a touch-up procedure later.
Open Surgical Repair
Traditional open surgical repair replaces the diseased segment through a midline abdominal incision. The aorta is clamped above and below the aneurysm, and a durable synthetic graft is sewn in to reinforce this weakened segment. That graft becomes part of your aorta.
Compared to EVAR, the long-term durability of an open repair is excellent, with fewer reinterventions once you are healed. Open repair works well when the anatomy is not suitable for EVAR. The trade-off is higher short-term surgical stress and a longer recovery window.
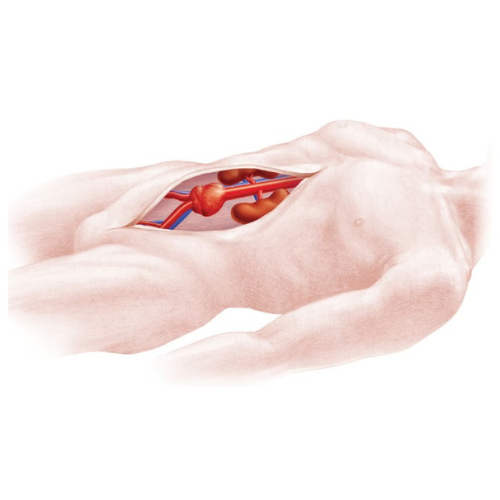
aneurysm.
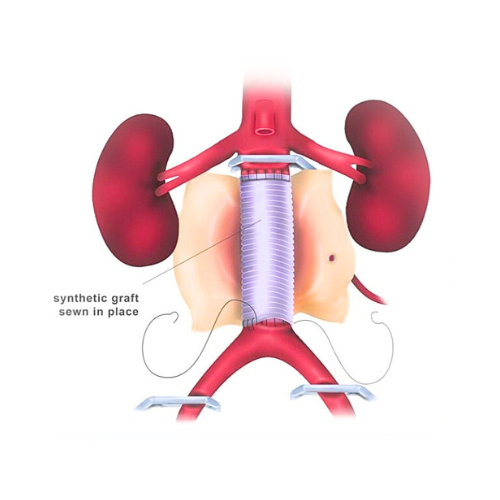
What to expect– Open surgical repair is a longer operation and the hospital stay is typically a few days while pain settles and the bowels recover. Recovery takes longer than with EVAR and builds steadily over several weeks.
EVAR vs Open Repair: How Your Vascular Surgeon Decides
Choice of abdominal aortic aneurysm surgery is guided by three questions. Does your anatomy suit a stent graft with a reliable seal. What does your baseline health suggest about the safety of each option. And what are your personal goals around recovery time and follow-up. Some people prefer the quickest recovery, others value the once-and-done stability of open repair.
There is no single “right” answer for everyone; the best approach is the one that matches your anatomy, your health and your priorities.
Conclusion
Living with an aortic aneurysm can feel overwhelming- like there a time bomb ticking away. The good news is that with the right advice, most patients can move forward with a clear plan. A good vascular surgeon can help you understand what your scan actually means, how urgent the situation is, and what options are most suitable for you.
If you would like a guided discussion, you can book a consultation with Dr. Darryl Lim, Vascular and Endovascular Surgeon. He is well-versed aortic aneurysm management, including the latest minimally invasive procedures like EVAR. His approach blends in-depth clinical knowledge with a focus on patient centred care. He will review your scans, explain your options in clear, simple language, and help you choose a plan that fits you best.










