Why These Bulging Leg Veins Matter
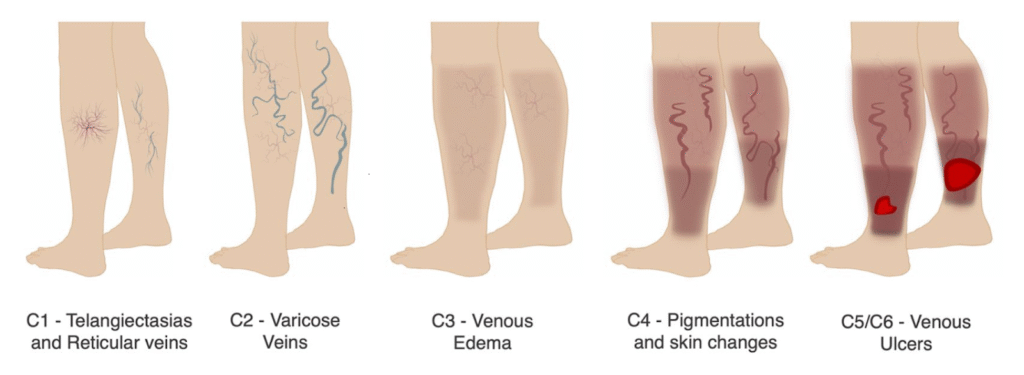
If you have noticed ropy, bluish-purple veins snaking across your calves, you are looking at varicose veins. They appear when the one-way valves inside the leg veins weaken, letting blood slide backwards and pool. In many people the problem is part of chronic venous insufficiency (CVI) – a broader circulation issue that can also cause spider veins, ankle swelling, skin discolouration or even non-healing ulcers.
While varicose veins can certainly dent confidence in shorts-weather Singapore, they are more than cosmetic.

Aching heaviness, night-time cramps and ankle puffiness can chip away at day-to-day comfort, making long ward rounds, shopping trips or school runs a chore. Left unchecked, the pressure may trigger eczema-like rashes or open sores around the ankle (venous ulcers).
Causes & Risk Factors

Long standing or sitting at work, lengthy MRT commutes, and even pregnancy can all nudge a “quiet” vein problem into full-blown varicose veins – but genetics has the first say. Put simply, you inherit vein walls that are either firm or slightly floppy; the floppier they are, the more easily the valves leak once life’s daily stresses pile on. The biggest culprits are:
- Family background – if a parent or sibling has ropey veins, your own risk nearly doubles.
- Hours on your feet (or seat) – nurses, teachers, security guards and office workers spend whole shifts fighting gravity or sitting motionless, slowing calf-pump flow.
- Hormonal surges and pregnancy – rising progesterone relaxes vessel walls, and nine months of extra blood volume stretches them further.
- Ageing – with time, the collagen scaffold inside the vein thins and valves lose their spring.
- Weight & inactivity – added abdominal pressure plus a weak calf muscle pump accentuates blood pool.
- Potential triggers/accelerators– smoking, a past deep-vein thrombosis, or long-term oestrogen therapy can all hasten the leakiness.
Knowing which factors apply to you helps Dr. Lim tailor both prevention (compression, exercise, weight control) and any treatment that follows.
Spotting the Symptoms
Varicose veins do not always scream for attention – many people are surprised when a routine check-up reveals just how much their legs have been compensating. Still, a few tell-tale clues often bubble up during a busy workday or after a long evening out:
- Dull, end-of-the-day ache or heaviness – that improves after you put your feet up.
- Night-time calf cramps – sudden cramps that jolt you awake, often easing when you stretch or massage the muscle.
- Morning-gone, evening-back swelling – calves or ankles puff up by late afternoon but look slimmer after a night’s rest.
- Itchy, fragile or brown-stained patches around the ankle – hint that blood has been pooling there for a while.
- Hard, painful cord-like lumps along a varicose vein – can signal a local clot or “phlebitis”.
If any of these warnings start to curb your daily activities, disturb your sleep, or dent your confidence in shorts weather, it is time to book a vein assessment.
Diagnosis: Looking Beneath the Surface
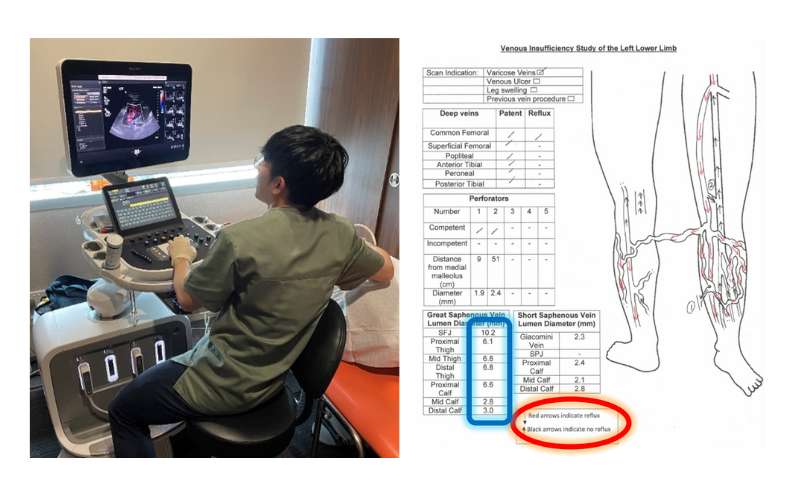
A quick look and a gentle palpation will confirm that those ropey veins are indeed varicose – but that surface check tells us little about why they formed (“root cause”) – namely which underlying venous trunks are “leaking”. To ascertain this diagnosis, we rely on a venous duplex ultrasound scan.
During this painless 20- to 30-minute scan, a trained sonographer traces every superficial vein from groin to ankle, measures each segment’s diameter, and watches in real time for backward flow (reflux). The deeper veins receive the same scrutiny, mainly to rule out hidden blood clots that could complicate any procedure.
This scan does three crucial things at once:
Provide the documentation insurers need for MediSave claims and Integrated Shield pre-authorisation.
Pinpoint the leaking trunks (long or short saphenous vein) so treatment targets the source, not just the surface.
Confirm the deep system is clear, ensuring it can take over once the faulty veins are closed.
Modern Treatment Options
The best news about vein treatment today? These keyhole procedures involve minimal downtime, with most patients returning to regular daily activities. We choose the least-invasive fix that still tackles the underlying reflux, often combining techniques so you leave with lighter legs and better skin.
| Treatment | Ideal for | How it works (and feels) |
| Lifestyle tweaks & compression stockings | Mild aching, pregnancy, long-haul flights | Graduated compression, brisk walks, and leg elevation ease symptoms but don’t erase the visible veins. Perfect as a first step or while you’re expecting. |
| Endovenous Radiofrequency Ablation (RFA) | Leaking long or short saphenous trunks with obvious bulging veins | A catheter gently heats the vein wall to about 120 °C. The faulty vein collapses and is reabsorbed by body over time, blood reroutes to healthy veins. Procedure time ~20 minutes per leg. |
| ClariVein® Pharmacomechanical Ablation | Leaking long or short saphenous trunks – “no-heat” treatment of the segments of these veins in close proximity to nerves | A rotating wire plus a low-dose sclerosant irritates and closes the vein shut. Most describe it as a mild vibration rather than pain. |
| Mini-phlebectomy (ambulatory phlebectomy) | Large, lumpy varicose veins that remain after trunk closure | 2-3 mm nicks are made and the diseased vein segments gently teased out; generally no stitches needed, only paper strips. Bruising fades in two weeks. |
| Sclerotherapy | Spider veins and small reticular veins (no underlying leaky vein trunks) | A fine needle delivers a foam or liquid solution that seals the vein from the inside. Done in the clinic in 30-60 minutes; you may need more than one session for optimal results. |
| VeinGogh® Ohmic Thermolysis | Smaller spider veins, residual “spider” veins after sclerotherapy | A hair-thin probe delivers a quick current burst, instantly coagulating the vessel. Feels like a brief pin-prick (somewhat similar to lasers). |
Most treatment plans consist of a combination of techniques- eg trunk-closing technique (eg RFA) with finishing touches (eg sclerotherapy or mini-phlebectomy) so both the root cause and the visible varicose/spider veins are tackled in a single sitting.
Need an expert vascular opinion for your Varicose Veins?
Book an appointment with Dr. Darryl Lim today and get a personalized treatment plan.

Cost of Treatment in Singapore – At a Glance
We know medical bills can feel like a maze, so here’s a quick, plain-English guide. The table below lists the commonly used surgical codes for varicose vein procedures and the typical surgeon’s fee range, based on the latest Ministry of Health (MOH) fee-benchmark and the Table of Surgical Procedures (TOSP). Do keep in mind: the final bill also reflects things like case complexity, single-use surgical consumables, the anaesthetist’s fee, and the choice of hospital facility the surgery is performed in. If you are ever unsure, just ask – our team will walk you through an itemised estimate before anything is booked, so there are no surprises.
| Procedure (Typical Private Setting) | Surgical Code | Surgeon Fee Range* |
| Endovenous thermal ablation (one leg) | SD713V | $4,900 – $7,300 |
| Endovenous thermal ablation (both legs) | SD714V | $6,700 – $10,100 |
| Sclerotherapy | SD717V | $1,900 – $4,300 |
| Mini-phlebectomy/Varicose vein stripping | SD808V | $2,600 – $4,300 |
* MOH surgeon-fee benchmarks effective 1 January 2025. Prices are in SGD, and are not inclusive of hospital facility, surgical consumable, anaesthetist fees and 9 per cent GST.
Consultation Fees with Dr. Darryl Lim
Novena Vascular & Varicose Vein Centre (Mount Elizabeth Novena Hospital Specialist Centre)
| Appointment type | Fee (SGD) | What’s included |
| Appointment type | $200 (Up to $250 – $300, depending on length or complexity) | Full history, physical examination, review of any existing scans, and a discussion of investigation or treatment options |
| Follow-up consultation | $130 – $160 | Progress review, wound or scan check, adjustment of treatment plan, and writing any referral letters (if required) |
Tip: If you need a same-day duplex ultrasound, we can often arrange it straight after your consultation so you only make one trip. Just let our team know when you book.
Will Insurance Help Pay for Varicose Vein Treatment?
Yes – most of the time. Once a duplex ultrasound shows significant reflux (“leaky valves”), the major Integrated Shield Plans usually recognise the procedure as medically necessary. How much they cover hinges on your plan tier and whether you have a rider, but many patients discover that their share is limited to the MediSave portion or a modest co-insurance payment.
Here is the simplest path to clarity:
- Send us your policy details. Our team will run the pre-authorisation and tell you the approved amount before you commit to anything.
- Touch base with your agent. They can confirm any rider or co-insurance nuances.
MediSave helps, too. The withdrawal limit is set by the MOH surgical table for the procedure performed, but it can offset a good chunk – or, in some cases, all – of the bill.
No private insurance? No problem. Just have a chat with our team – we’ll walk you through the available options and craft an affordable treatment plan that still delivers the care your legs deserve.
Life After Treatment
Most patients go home wearing a compression stocking, drive the next day, and return to regular activities within 48 hours. Bruising fades over two to three weeks; the aching, heavy sensation often resolves earlier. A follow-up scan at one week confirms the treated vein is sealed, and we discharge most patients after the three-month visit.
Why Patients Choose Dr Lim
Tucked inside Mount Elizabeth Novena Hospital, our vascular clinic is a one stop solution for all your vein needs. From the first ultrasound to your final sign-off, you deal directly with Dr. Darryl Lim, not a revolving cast of doctors.
Because Dr Lim also treats aortic aneurysms, peripheral vascular disease, and dialysis-access issues, he has an eye for wider circulation problems that might otherwise slip under the radar. If something else crops up, he can loop in your GP, endocrinologist, or cardiologist straight away, so all your vessels – and all your doctors – stay on the same page.
FAQ about Varicose Veins
Varicose veins are enlarged, twisted veins that are visible under the surface of the skin. They often appear in the legs and can cause discomfort, pain, or swelling.
Spider veins are smaller, more superficial veins that often appear as blue, purple, or red lines on the skin surface. They are typically not painful but can be cosmetically bothersome to some individuals.
Several factors contribute to the development of varicose and spider veins, including age, genetics, hormonal changes, pregnancy, obesity, and prolonged periods of standing or sitting.
While spider veins are generally harmless, varicose veins can sometimes lead to complications such as bleeding, blood clots, and ulcers. It is advisable to consult with a healthcare provider for diagnosis and treatment options.
Approximately half of the population has some form of venous disease while varicose veins affect one out of two people age 50 and older, and 15-25% of all adults. On average 18% of men and 25% of women develop varicose veins. Varicose veins are one of the most common venous issues affecting the world today.
Anyone can develop spider or varicose veins, but they are more common in those above 50 years old, females, individuals with a family history, and those with certain lifestyle factors like a high BMI, desk-bound work environments, or in occupations which require you to stand for long periods of time.
Here are some physical symptoms of varicose veins that make them easier to diagnose:
- Itchy or flaky skin around the affected vein, sometimes accompanied by a burning sensation,
- Feeling of heaviness or ache in the lower legs after standing or sitting for long periods of time (usually worse at end of day, with comparative relief in the morning),
- Muscle cramps or pain in the lower legs, and,
- Swelling around the ankles – the ankle area appears puffy and swollen, and the ankle bone may not be visible
Not all of these symptoms are present in the same person. However, if you fit the above description, or if you have one or more of these symptoms, it is likely you have varicose veins. These symptoms can take a toll on your quality of life, making it hard to do things like walking or even standing for long periods.
Fortunately, modern minimally-invasive surgical methods have made the treatment of varicose veins quick and easy. Feel free to reach out for a personalised assessment and consultation should you have any of the above concerns.
While not all people present with severe symptoms, varicose veins generally worsen over time. Initially, slight heaviness and discomfort in the affected leg will be felt. If untreated, this pain may increase and result in limitations in walking and cramping during the night. Eventually, varicose veins can lead to skin discolouration or open wounds (ulcers) around the ankles.
Your healthcare provider will usually diagnose these conditions based on a physical examination. Additional tests like ultrasound may be recommended to assess the presence of venous incompetency (reflux), and rule out other issues.
An ultrasound is the most common diagnostic test for varicose veins. Some patients may require a CT (Computed Tomography) scan of your abdomen may be indicated to evaluate for compression of your pelvic veins.
Treatment options may include lifestyle changes, compression stockings, minimally invasive procedures like sclerotherapy, radiofrequency ablation therapy, and surgical interventions like vein stripping.
Generally, spider veins are treated with less invasive methods like injection sclerotherapy or radiofrequency treatment. Spider veins usually require a few sessions of sclerotherapy to resolve.
Varicose veins may additionally require more extensive treatment like mini-stab avulsions (for removal) depending on their extent and severity.
Coverage varies by insurance provider and plan. It is essential to consult your insurance to determine what treatments are covered, especially since some treatments may be considered cosmetic.
Clinical results have been published documenting the success of Endovenous Radiofrequency Ablation, ClariVein and VenaSeal at above 90% and Sclerotherapy between 60-80%.
As with any medical treatment, each method has its own risks and benefits. Your surgeon will explore the most suitable treatment option, after a thorough assessment of your condition.
Sclerotherapy is commonly used to treat spider veins (small superficial veins) and has been used with safety and success since the 1930’s. This treatment is a non-surgical procedure, and can be performed in the outpatient clinic.
Using a very fine needle, a solution is injected into the vein. This solution causes the vein walls to stick together and eventually close. The obliterated vein is absorbed by the body over time.
Following sclerotherapy, there is very little to no downtime. Patients will be required to wear a compression stocking for the next week. They can return to work or carry on with normal activities straight away. Some patients may experience gentle bruising at the treated area, especially those with thin and lighter skin.
Patients should wait at least three months after pregnancy before being treated for venous insufficiency. Patients who have suppressed immune systems, deep vein thrombosis, and patients who are immobile (ie cannot walk or move around), are generally not good candidates for treatment and will require further evaluation to assess their suitability.
Recovery depends on the treatment method used. Minimally invasive treatments usually have shorter recovery times. Most patients will be able to walk on the same day after their surgery. Traditional open surgical treatments (eg open stripping of vein) may require a longer period for full recovery.
Yes. There is a possibility that new varicose or spider veins may develop over time even after successful treatment, particularly if underlying risk factors are not addressed. Risk of recurrence is usually around 5-10%.
This depends on the type of treatment you undergo. For minimally invasive treatments, most people can return to normal activities relatively quickly in a day or two. Vigorous exercise is usually not recommended till 2 weeks post-surgery. Traditional open surgical treatments may require a longer period for full recovery.
Most treatments aim to reduce the appearance and symptoms of varicose and spider veins significantly, but results can vary from person to person.
While many people seek treatment for cosmetic reasons, treatment can also alleviate symptoms like pain, swelling, and itching associated with varicose veins.
You can schedule a consultation by:
- Calling our clinic at +(65) 6694-2282,
- Leaving us a Whatsapp message +(65) 9727-0788,
- Emailing contact@drdarryllim.com, or
- Using our contact form
During your first consultation, your vascular surgeon will examine your veins, discuss your symptoms, go over your medical history, and possibly recommend additional tests. A personalized treatment plan will then be discussed.
Varicose veins are mainly caused by venous reflux- when vein valves weaken and blood flows backward, increasing pressure in the leg veins. Ageing, pregnancy, obesity, prolonged sitting or standing, and inactivity can all raise your risk.
No, varicose veins don’t go away on their own and usually get worse over time. Minimally invasive vein treatments can help relieve symptoms and significantly improve their appearance.
Berries- like blueberries, cherries, and blackberries- are great for varicose veins. They’re rich in antioxidants and flavonoids, which help strengthen blood vessels, reduce inflammation, and improve circulation.
Minimally invasive treatments like radiofrequency ablation (RFA) or sclerotherapy are safe and effective options. They involve little downtime, have a low risk of complications, and offer reliable relief from symptoms with good cosmetic results.
Minimally invasive treatments like radiofrequency ablation (RFA) or sclerotherapy are safe and effective options. They involve little downtime, have a low risk of complications, and offer reliable relief from symptoms with good cosmetic results.
Not always. Varicose veins are common and often caused by genetics, ageing, or lifestyle factors. While they can cause discomfort, they don’t always mean poor health. However, they may indicate underlying vein issues and should be checked if symptoms worsen.
You can’t completely fix varicose veins on your own, but lifestyle changes like wearing compression stockings, staying active, and elevating your legs can help manage symptoms. For lasting results, medical treatments like vein ablation or sclerotherapy are usually recommended.










