Deep Venous Arterialization (DVA)
Peripheral Arterial Disease (PAD) is a common circulatory problem where narrowed arteries reduce blood flow to the limbs.
Up to 20% of patients with limb-threatening ischemia have arterial disease that is not amenable to traditional revascularization techniques, and are described as having a “desert foot”. This condition is more common in patients with diabetes and end-stage kidney disease- they often have severely calcified and blocked vessels extending below the ankle.
When PAD progresses to a critical level, it can lead to severe limb ischemia (oxygen-starved), which commonly manifests as intense pain, non-healing wounds, and gangrene. These patients may eventually require to a major amputation above the ankle.
Deep Venous Arterialization (DVA) emerges as a cutting-edge alternative. This innovative procedure aims to restore blood flow to the affected limbs, offering hope to those who might otherwise face amputation.

Understanding Deep Venous Arterialization (DVA)
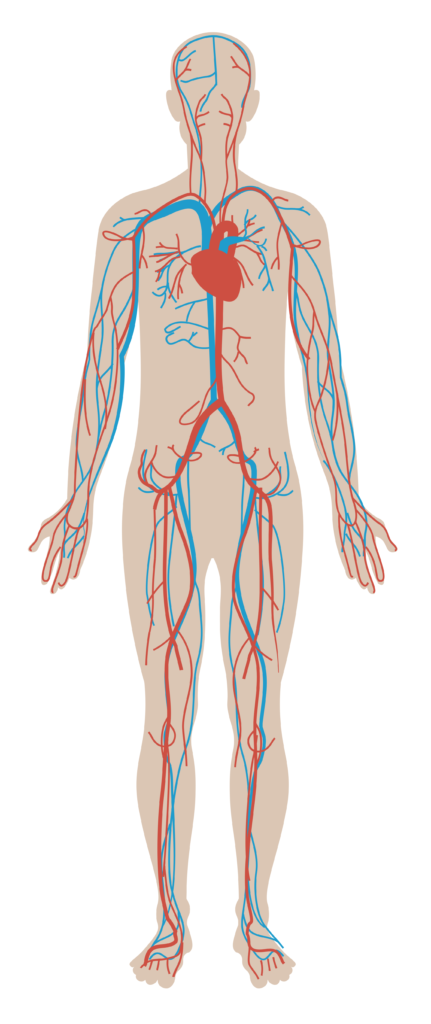
Our body comprises two main vascular systems: arteries and veins. Arteries (red) are responsible for carrying blood from the heart to the rest of the body, while veins (blue) return blood back to the heart.
DVA is a surgical technique that reroutes blood flow from the arteries directly into the deep veins of the leg or foot. By bypassing the blocked or diseased peripheral arteries, DVA allows arterial blood to flow through the venous system, reaching the oxygen-starved tissues. This process revitalizes the tissues, encouraging healing of ulcers and reducing pain.
The Procedure - how it is performed
DVA involves several steps, performed under general or regional anaesthesia:
1. Vessel access and examining the arteries:
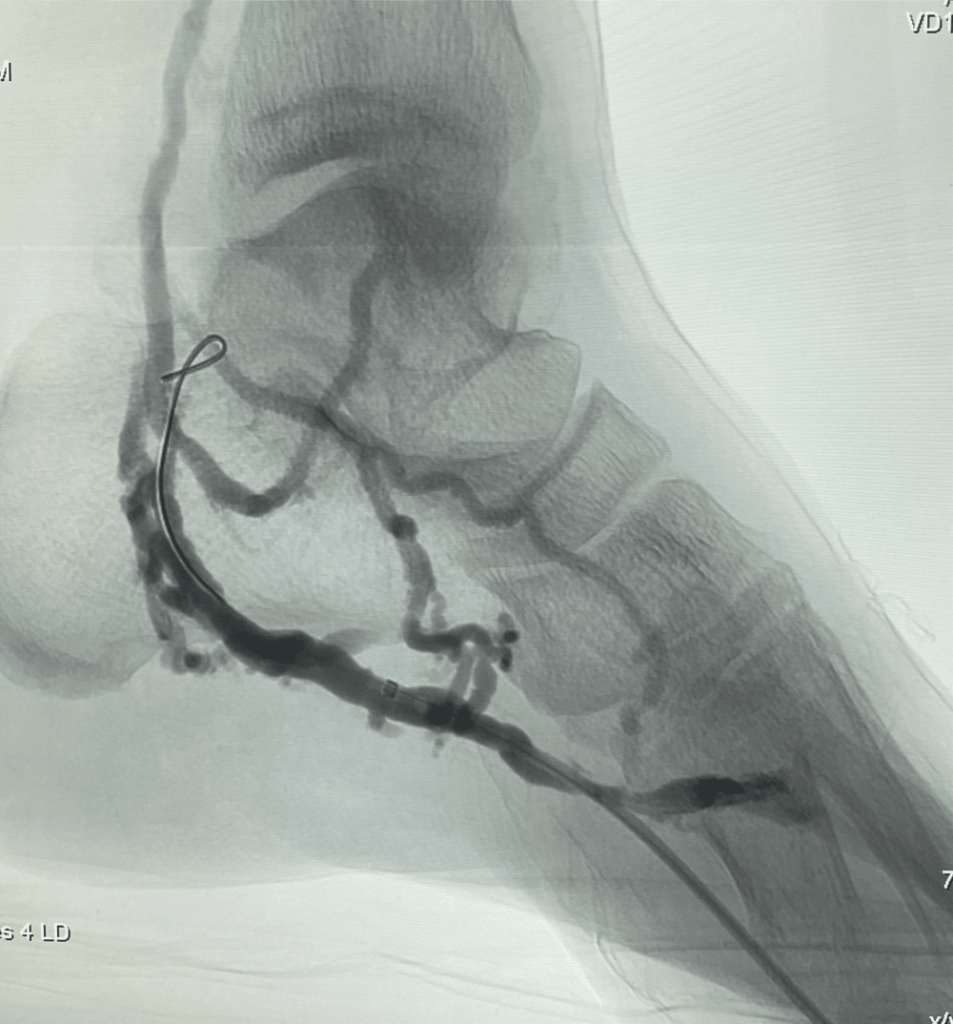
First, a mini-incision is made in the groin to access the femoral artery. A diagnostic angiogram is then performed- this is a type of X-ray that shows how blood flows to the foot.
The angiogram shown here demonstrates sparse contrast flow down to the foot, indicative of severe blockage of the arteries below the ankle. This condition is commonly referred to as a “desert foot”.
2. Accessing the foot veins
Using ultrasound for guidance, a vein in the foot (usually the lateral plantar vein) is punctured, and another angiogram is performed. This helps evaluate if the veins in the foot are suitable for the Deep Venous Arterialization procedure.
3. Creation of a new pathway to the foot
A thin tube (catheter) and wire are carefully guided up from the veins in the foot, and positioned adjacent to a healthy segment of artery below the knee.
Using a specialised tool (re-entry crossing device), a needle at the device tip punctures through the artery wall into the adjacent vein. This crucial step requires proper positioning and technique. Once within the vein, the wire is then manipulated down towards the veins in the foot.
open in full screen to view in full
4. Creation of an Arteriovenous Fistula and re-establishing blood flow to the foot
This newly created pathway is then gradually paved open with balloon angioplasty and stenting, creating an arteriovenous fistula in the process- this results in the re-routing of blood flow from the arteries into the veins of the foot.
This innovative procedure helps deliver arterial blood to the foot via the venous system.
open in full screen to view in full
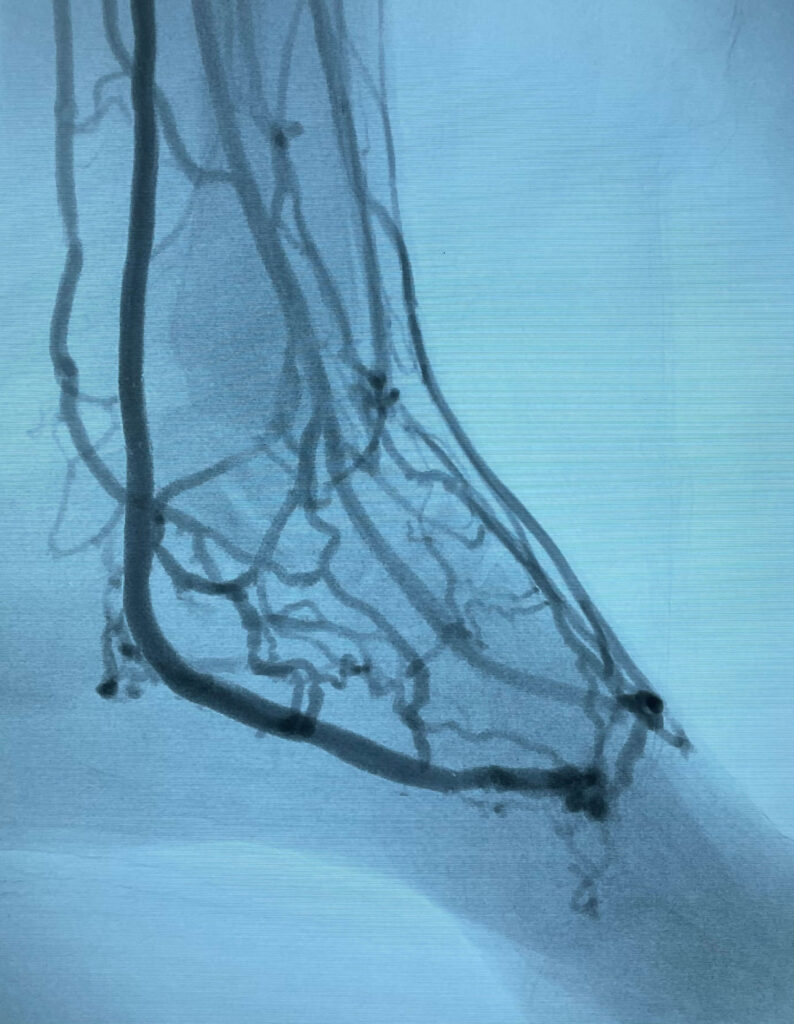
5. Checking the results
A final angiogram is performed. This angiogram shows successful diversion of blood flow to the foot, alleviating the circulatory blockage, and relieving the foot of ischemia.
The only device currently on the market which is purpose built for performing a DVA (also known as TADV- transcatheter arterialization of the deep venous system) is the LimFlow system. Apart from slight modifications, the steps involved are largely similar, and video below shows this procedure in greater detail.
Who Can Benefit from DVA?
Patients with critical limb ischemia (CLI) resulting from PAD, who cannot undergo traditional revascularization procedures due to blocked arteries being too severely diseased for bypass or conventional angioplasty. It is a viable last-resort option for patients facing potential lower limb amputation.
Benefits of DVA
- Limb Salvage: DVA can significantly reduce the risk of limb amputation by restoring blood flow to ischemic limbs.
- Pain Reduction: By improving blood circulation, DVA can alleviate the severe pain associated with CLI.
- Healing of Ulcers: Enhanced blood flow promotes the healing of non-healing wounds and ulcers.
- Improved Quality of Life: Patients can experience improved mobility and a better overall quality of life.
Recovery and Aftercare
Postoperative care is crucial for the success of DVA. Patients may need to stay in the hospital for at least few days for monitoring- this depends on the individual patient’s underlying medical problems and disease severity. Following discharge, regular follow-up appointments are necessary to assess the functionality of the newly created vascular circuit and the overall health of the limb. Rehabilitation and walking exercises are often recommended to enhance the benefits of the procedure.
Conclusion
Deep Venous Arterialization represents a promising frontier in the treatment of critical limb ischemia for patients with severe peripheral arterial disease. By offering a novel way to restore blood flow to ischemic tissues, DVA provides hope for those at risk of amputation, fostering improved outcomes and a better quality of life.
Dr. Lim is among a small handful of surgeons in the region who have the expertise to perform this procedure. If you or a loved one are facing the challenges of peripheral arterial disease, do reach out for a consult to determine if DVA could be a suitable treatment option.
FAQ's about DVA
Deep Venous Arterialization is an innovative endovascular procedure designed to treat severe Peripheral Arterial Disease (PAD) and Critical Limb Ischemia (CLI) by rerouting blood flow from arteries to the deep veins in the leg or foot, bypassing blocked arteries to restore blood flow to ischemic tissues
- Candidates for DVA typically include patients with critical limb ischemia resulting from severe peripheral arterial disease, who are not suitable for traditional revascularization methods such as bypass surgery or angioplasty due to extensive arterial blockages or damage.
- This can occur in up to 20% of patients with limb-threatening ischemia, and these patients are described as having a “desert foot”.
- DVA aims to restore adequate blood flow to the affected limbs by rerouting blood from the arteries into the veins.
- This promotes healing of ulcers, reducing pain, and ultimately decreasing the risk of amputation by revitalizing ischemic tissues that are at risk due to insufficient blood supply.
While DVA offers significant benefits, it carries risks like any surgical procedure, including infection, bleeding, and the potential for deep vein thrombosis (DVT) or heart failure. The specific risks depend on individual patient factors (like underlying medical conditions) and the complexity of the procedure.
- The technical success rate (ie successful execution of surgery) should be more than 95% in experienced hands.
- However, it is important to understand that the success of subsequent wound healing and limb salvage depends on several other factors such as the patient’s overall health and extent of ischemia/wounds before the procedure. The landmark PROMISE II Trial published in the New England Journal of Medicine (NEJM) demonstrated a 76% limb salvage rate with DVA.
The recovery period can vary from patient to patient, but patients may need to stay in the hospital for at least a few days post-surgery for monitoring. Full recovery, including wound healing and rehabilitation, may take several weeks to months, with regular follow-up appointments to ensure successful adaptation to the new blood flow pathway.
DVA does not “cure” PAD but is a treatment aimed at managing its most severe complications, such as critical limb ischemia, by restoring blood flow to areas affected by arterial blockages, thus alleviating symptoms and reducing the risk of limb loss.
Determining if DVA is the right treatment option involves a comprehensive evaluation by an experienced vascular surgeon, who will consider your medical history, the severity of your PAD and CLI, and your overall health to recommend the best treatment approach.
- Alternatives to DVA may include traditional revascularization methods like angioplasty, stenting, or bypass surgery, as well as conservative treatments such as medication and lifestyle changes. In some cases, limb amputation may be considered if other treatments are not viable or effective.
- Do note that DVA is not typically performed as a first-line treatment option for patients with peripheral arterial disease presenting for the first time. It is usually only considered when conventional surgical modalities have been unsuccessful.
- Deep Venous Arterialization involves complex endovascular intervention, and is best performed by vascular surgeons who possess sufficient experience with the procedure. Dr. Lim is among a small handful of surgeons in Asia to be adept at performing this procedure, as well as managing DVA patients after the procedure.
- If you or a loved one are facing the challenges of peripheral arterial disease, do reach out for a consult to determine if DVA could be a suitable treatment option.