Radiofrequency Ablation
What is Radiofrequency Ablation?

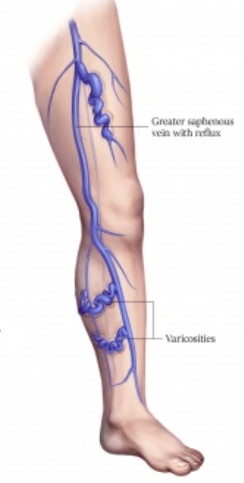
Radiofrequency Ablation (RFA) is a minimally invasive procedure designed to treat varicose veins and venous reflux disease. By using carefully controlled heat to seal off unhealthy veins, RFA directs blood flow toward healthier vessels, effectively reducing symptoms and improving the overall appearance of the legs. This approach is often preferred over traditional vein stripping surgeries due to its high success rate, relatively minimal discomfort, and quicker recovery time.
Why is Radiofrequency Ablation needed?
RFA treats underlying venous reflux disease, a condition characterized by backward blood flow due to malfunctioning valves in the leg veins. This disease can cause pain, swelling, and the development of varicose and spider veins. RFA uses heat to seal malfunctioning veins, allowing blood to be redirected to healthier ones.
Pre-Procedural Evaluation
Before scheduling an RFA procedure, you will undergo a thorough evaluation to pinpoint which veins are contributing to your venous reflux disease. An ultrasound scan provides a detailed view of your leg veins and helps the vascular surgeon identify their precise condition and severity. In some instances, a Computed Tomography (CT) scan will be required if there is suspicion of compression of your larger iliac veins in your abdomen. This pre-procedural assessment ensures that the treatment can be tailored to your specific needs, maximizing the likelihood of successful treatment.
How is the Radiofrequency Ablation procedure performed?
On the day of your Radiofrequency Ablation, you will typically be asked to avoid eating or drinking for at least six hours beforehand, especially if you are receiving general or spinal anesthesia. Some patients opt for local anesthesia with sedation, which can also be effective for keeping you comfortable.
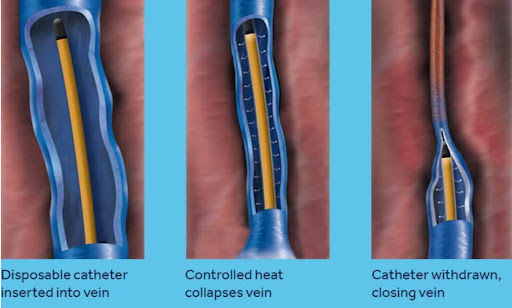
Once you’re prepared, a small incision—often above the knee—is made to insert a specialized catheter into the affected vein. Ultrasound guidance ensures precise positioning. A fluid mixture containing diluted local anesthetic, known as tumescent anesthesia, is then infused around the vein to provide additional pain relief and safeguard surrounding tissues. Radiofrequency energy is applied through the catheter, gently heating the vein walls so that they collapse and seal shut, eliminating the backward flow of blood in the treated vein. The procedure itself generally takes between 30 and 60 minutes, and additional treatments (such as removing bulging varicose veins or treating spider veins) can sometimes be performed during the same session.
On the procedure day, patients are advised to abstain from eating and drinking for at least 6 hours beforehand. The procedure is typically performed under general or spinal anesthesia to enhance patient comfort, although local anesthesia with sedation is also an option.
What to expect after the procedure?
Most patients are discharged by the following morning, though some return home the same day. You will be encouraged to start walking soon after the procedure to support healthy circulation and reduce the risk of complications. While everyone heals at a slightly different pace, many people resume normal activities by the next day. Exercise can be resumed after about two weeks, while wearing a compression stocking for one to two weeks helps reduce swelling and promotes faster healing.
What are the risks associated with Radiofrequency Ablation?
Although Radiofrequency Ablation is considered safe and effective, like any medical procedure, it carries some potential risks. Minor bruising or swelling around the incision sites is relatively common but typically short-lived. More serious issues, such as skin burns or nerve injury causing numbness, are quite rare. There is also a small risk—around one percent—of developing Deep Vein Thrombosis (DVT). Additionally, a five to ten percent chance exists that varicose veins may recur due to progressive changes in the vein structure over time. Nevertheless, RFA remains a popular choice for patients seeking reliable relief from venous reflux disease.
Conclusion
Radiofrequency Ablation offers a less invasive alternative to traditional vein surgery, enabling patients with varicose veins and venous reflux disease to experience meaningful relief and improved quality of life. If you’ve been dealing with leg pain, swelling, or unsightly veins, reach out to schedule a consultation and discuss whether Radiofrequency Ablation is the right option for you.
This information is provided as a general guideline and should not replace professional medical advice. Always consult with your healthcare provider for personalized recommendations.
FAQ's about Radiofrequency Ablation
RFA is performed under anesthesia, where a catheter is inserted into the damaged vein through a small incision, and radiofrequency energy is administered to heat and seal the vein.
Patients generally experience minimal discomfort during RFA due to the use of anesthesia and can expect minimal pain post-procedure.
Most patients can return to their regular activities within a day and resume strenuous activities after 2 weeks.
RFA is a safe and minimally invasive procedure with rare risks and side effects, which are usually minor and temporary.
Potential side effects include minor bruising, swelling, rare risk of skin burns, or discoloration, and extremely rare risks include Deep Vein Thrombosis (DVT) and nerve injury.
RFA is utilized to address the larger underlying veins whose malfunction leads to the manifestations of venous reflux. Spider veins are typically addressed by other treatment modalities, such as injection sclerotherapy.
Without addressing the underlying venous reflux, the risk of spider veins recurring is much higher if only injection sclerotherapy is used. Consequently, these two procedures are often performed concurrently.
Radiofrequency Ablation has a high success rate in treating venous reflux disease, with a low recurrence rate of varicose veins.
While the treated (ablated) vein segments rarely recur, the formation of new veins over time can lead to recurrence.
RFA is often covered by insurance when it is medically necessary due to symptoms, but coverage may vary, and it’s recommended to consult with your insurance provider.
The procedure typically takes about 30 to 60 minutes, depending on the number of veins being treated.
Patients are encouraged to start walking shortly after the procedure to promote blood flow and aid in the healing process.
Yes, wearing compression stockings is usually recommended for 1-2 weeks post-procedure to reduce swelling and improve healing.
While RFA is effective, there is a 5-10% possibility of recurrence of varicose veins due to the progression of venous disease.
Patients are usually advised to abstain from eating and drinking for at least 6 hours before the procedure.
Yes, RFA is typically an outpatient procedure. The procedure can be performed in a day surgery centre, and most patients are discharged the next morning.
Most patients are encouraged to start walking shortly after the procedure. Depending on the extent of the treatment, the majority can typically resume work and regular activities within a few days post-procedure
Indeed, several contemporary, minimally invasive options are available for the treatment of varicose veins and venous reflux.
The choice of treatment is multifaceted, depending on the patient’s symptoms, vein anatomy, cost, and your surgeon’s preferences.
After a thorough clinical assessment, Dr. Lim will tailor an individualized treatment plan to address your specific varicose veins condition effectively.


