Blocked arteries are a significant health concern, often leading to severe complications such as heart attacks, strokes, and other life-threatening conditions. When arteries become narrowed or blocked due to plaque buildup, it can severely restrict blood flow, leading to various health issues. One of the most effective treatments for restoring blood flow in these blocked arteries is a combination of angioplasty and stent placement. This minimally invasive procedure has become a cornerstone in the management of cardiovascular and peripheral arterial diseases.
Understanding Arterial Blockages
Arteries are vital blood vessels that carry oxygen-rich blood from the heart to the rest of the body. Over time, these arteries can become narrowed or blocked due to the buildup of fatty deposits known as plaque—a condition known as atherosclerosis. When this occurs, the flow of blood is restricted, leading to symptoms such as chest pain (angina), leg pain when walking (claudication), or even more severe consequences like heart attacks or strokes.
Atherosclerosis can affect any artery in the body, including those in the heart (coronary arteries), neck (carotid arteries), and limbs (peripheral arteries). The goal of treatment is to restore adequate blood flow and prevent further complications.

What is angioplasty?
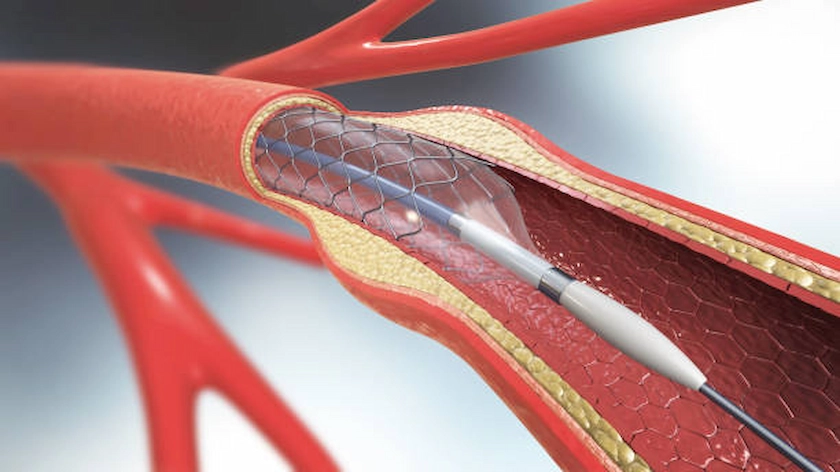
Angioplasty is a minimally invasive procedure designed to open up blocked or narrowed arteries. During the procedure, a catheter with a small balloon at its tip is inserted into the artery and guided to the site of the blockage. Once in position, the balloon is inflated, pressing the plaque against the artery walls and widening the artery to improve blood flow.
The Role of Stent Placement
While angioplasty alone can effectively open a blocked artery, there is a risk that the artery may narrow again over time—a process known as restenosis. To reduce this risk, a stent is often placed during the procedure. A stent is a small, mesh-like tube that acts as a scaffold, keeping the artery open and maintaining blood flow.
There are different types of stents, including bare-metal stents and drug-eluting stents. Drug-eluting stents are coated with medication that helps prevent the artery from narrowing again, making them particularly effective in reducing the likelihood of restenosis.
The Procedure: What to Expect
Angioplasty and stent placement are typically performed under regional or general anesthesia. The procedure usually takes about one to two hours, depending on the complexity of the blockage.
A small incision is made in the groin, through which the catheter is inserted and guided to the blocked artery. Using X-ray imaging, the surgeon carefully positions the balloon and stent at the site of the blockage. After the balloon is inflated and the stent is placed, the balloon is deflated and removed, leaving the stent in place to keep the artery open.
After the procedure, you will be monitored for a few hours to ensure there are no complications. Most patients can return home the same day or the next day, depending on their overall health and the complexity of the procedure.
Benefits of Angioplasty and Stent Placement
The primary benefit of angioplasty and stent placement is the immediate restoration of blood flow to the affected area. This can relieve symptoms such as chest pain, leg pain, and shortness of breath, significantly improving your quality of life. Additionally, by restoring blood flow, the procedure helps prevent more serious complications, such as heart attacks or the need for limb amputation in severe cases of peripheral artery disease.
Another advantage is that angioplasty and stent placement are less invasive than traditional surgery, which means a shorter recovery time and less risk of complications. Most patients can resume normal activities within a few days to a week after the procedure.
Risks and Considerations
Like all medical procedures, angioplasty and stent placement come with risks. These may include bleeding, infection, or a reaction to the contrast dye used during the procedure. In rare cases, the artery can be damaged or the stent may move from its original position. There is also a small risk of blood clots forming around the stent, which could lead to a heart attack or stroke.
However, these risks are relatively low, and the procedure is generally considered safe, especially when performed by an experienced vascular surgeon. It’s important to discuss these risks with your healthcare provider to make an informed decision about your treatment.
Long-term management and follow-up
While angioplasty and stent placement can effectively open blocked arteries, they are not a cure for atherosclerosis. Long-term management is crucial to prevent further blockages and maintain the health of your arteries. This includes lifestyle changes such as quitting smoking, eating a healthy diet, exercising regularly, and taking medications to control blood pressure, cholesterol, and blood sugar levels.
Regular follow-up visits are also essential to monitor the condition of your arteries and ensure that the stent is functioning properly. Imaging tests such as ultrasound or angiography may be used to check for signs of restenosis or other complications.
For a deeper understanding of how these procedures fit into the overall management of cardiovascular and peripheral arterial diseases, explore how our vascular treatments are tailored to each patient’s unique needs.
Conclusion
Angioplasty and stent placement are powerful tools in the fight against blocked arteries, offering a minimally invasive solution to restore blood flow and prevent serious complications. If you are experiencing symptoms of arterial blockages or have been diagnosed with atherosclerosis, this procedure may be an effective treatment option for you.
Understanding the details of the procedure and its role in managing your condition is key to making informed decisions about your health. For more insights into how we approach the care of vascular conditions, our treatment strategies are designed to ensure comprehensive and personalized care.
Your vascular health is vital, and with the right treatment and management, you can significantly improve your quality of life and reduce the risk of future complications.

















