Varicose veins are those twisted, bulging veins that often appear blue or dark purple, typically on the legs. These veins develop when the valves inside them don’t work properly, causing blood to pool instead of flowing smoothly back to the heart. This can lead to discomfort, swelling, and more serious health problems if left untreated. Luckily, there are many effective treatments available today.

Understanding Varicose Veins
Varicose veins result from a condition called venous insufficiency. This happens when the valves in your veins fail, allowing blood to accumulate. Various factors contribute to this condition, including genetics, aging, prolonged standing or sitting, obesity, and pregnancy. People with varicose veins often experience symptoms that range from cosmetic concerns to pain, swelling, and even ulcers.
Current Treatment Options
Endovenous Radiofrequency Ablation (RFA)
One of the modern methods to treat varicose veins is Endovenous Radiofrequency Ablation (RFA) . During this procedure, a thin catheter is inserted into the vein under ultrasound guidance. Radiofrequency energy is then used to heat and seal the vein, redirecting blood flow to healthier veins. This technique is minimally invasive, has a short recovery time, and can be done as an outpatient procedure, making it a highly effective option.
Clarivein Mechanochemical Ablation (MOCA)
Another innovative treatment is the Clarivein Mechanochemical Ablation (MOCA), which uses a rotating catheter and a sclerosant solution to collapse and seal the vein without heat. This reduces the risk of thermal injury. MOCA is particularly suitable for sealing veins below the knee, offering less pain and a quicker recovery.
Ultrasound-Guided Foam Sclerotherapy
Ultrasound-Guided Foam Sclerotherapy involves injecting a foam sclerosant into the vein under ultrasound guidance. The foam causes the vein to close and gradually disappear. This method is minimally invasive and effective for smaller veins, providing a quick and simple solution.
VenaSeal (Medical Adhesive or “Super Glue”)
VenaSeal is another advanced treatment option where a medical adhesive is used to seal the vein. The body then absorbs the sealed vein over time. This procedure is minimally invasive, does not require compression stockings after treatment, and allows for a quick recovery.
Ambulatory Phlebectomy
Ambulatory Phlebectomy is a procedure where small incisions are made to remove varicose veins close to the skin surface. This method is effective for immediate removal of big bulging surface veins, leaves minimal scarring, and is usually performed at the same time as the venous reflux procedure.
Compression Therapy
Compression therapy involves wearing compression stockings to improve blood flow and reduce symptoms. It is also used post-operatively for 2-4 weeks to reduce bruising and aid in a faster recovery. Do note that the use of compression stockings alone does not definitively treat the underlying venous reflux.
Lifestyle Changes
Making certain lifestyle changes can significantly improve vein health and help manage varicose veins. Regular exercise is crucial as it improves circulation. Maintaining a healthy weight reduces the pressure on your veins, and avoiding prolonged periods of standing or sitting helps prevent blood from pooling in the legs.
Post-Treatment Care
After undergoing treatment for varicose veins, proper post-treatment care is essential for optimal recovery. Wearing compression stockings can help reduce swelling and aid in recovery. Elevating your legs can also improve circulation and reduce swelling. Staying hydrated and maintaining a balanced diet supports overall vein health. Regular follow-ups with your healthcare provider are important to monitor your progress and prevent recurrence.
Risks and Considerations
While modern treatments for varicose veins are generally safe, there are potential risks to be aware of. These include infection at the treatment site, rare occurrences of nerve damage, recurrence of varicose veins, and allergic reactions to sclerosants or adhesives. Your vascular surgeon will have a more detailed discussion with you about this prior to any procedure.
Struggling with Varicose Veins?
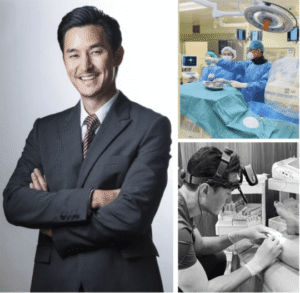
Explore safe and effective treatment options with Dr. Darryl Lim.
Conclusion
Varicose veins can really impact your daily life, but the good news is that there are many effective, minimally invasive treatments available today. If you’re looking for personalized advice and the latest treatment options, visiting Dr. Darryl Lim’s clinic might be a great next step. With specialized care and advanced techniques, you can find relief from varicose veins and improve your vascular health.