Peripheral Vascular Disease (PVD) is a serious circulatory condition that affects millions of people, particularly those with diabetes. PVD occurs when the blood vessels outside of your heart and brain, particularly those in the legs, become narrowed or blocked due to the buildup of fatty deposits, known as plaque. This condition can lead to reduced blood flow, causing pain, tissue damage, and an increased risk of serious complications. For individuals with diabetes, the risk of developing PVD is significantly higher, making it crucial to understand the connection between diabetes and PVD and to take proactive steps to manage both conditions.

Understanding peripheral vascular disease
Peripheral Vascular Disease refers to the narrowing or blockage of blood vessels that supply blood to the limbs, most commonly the legs. This reduction in blood flow can lead to a range of symptoms, including leg pain when walking, numbness, coldness in the feet or lower legs, and in severe cases, non-healing sores or ulcers. PVD is often a result of atherosclerosis, a condition in which plaque builds up on the walls of the arteries, causing them to harden and narrow.
While PVD can affect anyone, it is particularly common among individuals with diabetes. This is because diabetes can accelerate the process of atherosclerosis, leading to earlier and more severe blockages in the arteries.
How Diabetes Increases the Risk of PVD
Diabetes significantly increases the risk of developing peripheral vascular disease for several reasons:
- Accelerated Atherosclerosis: High blood sugar levels in people with diabetes can damage the inner lining of the blood vessels, making them more susceptible to the buildup of plaque. Over time, this plaque hardens and narrows the arteries, reducing blood flow to the limbs and increasing the risk of PVD.
- Increased Blood Viscosity: Diabetes can cause changes in blood viscosity, or thickness, making it more difficult for blood to flow through narrowed arteries. This increased blood viscosity further exacerbates the risk of blockages and reduces the effectiveness of circulation, particularly in the smaller blood vessels of the legs and feet.
- Nerve Damage (Neuropathy): Diabetes can lead to nerve damage, known as neuropathy, which affects the nerves that control blood flow and sensation in the limbs. Neuropathy can make it difficult to detect early symptoms of PVD, such as pain or coldness in the legs, leading to delayed diagnosis and treatment.
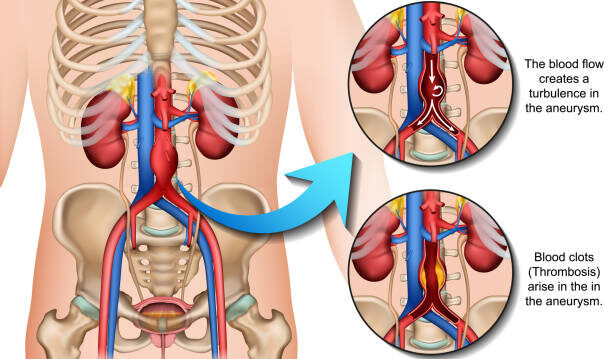
- Increased Risk of Blood Clots: People with diabetes are more prone to developing blood clots, which can further obstruct blood flow in already narrowed arteries. This increases the likelihood of severe complications, such as critical limb ischemia, where blood flow is so restricted that it leads to tissue death and the potential need for amputation.
Recognizing the Signs of PVD in Diabetics
For individuals with diabetes, it is particularly important to be vigilant about the signs and symptoms of peripheral vascular disease. Early detection and treatment are key to preventing serious complications. Common signs of PVD include:
- Leg Pain During Activity (Claudication): Pain, cramping, or fatigue in the legs or hips during walking or exercise that goes away with rest.
- Numbness or Weakness: A feeling of weakness or numbness in the legs, often accompanied by a sensation of heaviness.
- Coldness in the Lower Legs or Feet: The affected limb may feel colder than the rest of the body due to reduced blood flow.
- Sores or Wounds That Won’t Heal: non-healing sores or ulcers on the legs or feet, which can lead to infections and further complications.
- Changes in Skin Color: The skin on the legs or feet may become pale, blue, or shiny, indicating poor circulation.
If you experience any of these symptoms, especially if you have diabetes, it is crucial to seek medical attention promptly. Early diagnosis of PVD can lead to more effective treatment and reduce the risk of complications.
Managing the Risk of PVD in Diabetics
While diabetes increases the risk of peripheral vascular disease, there are several steps you can take to manage this risk and maintain vascular health:
- Blood Sugar Control: Keeping your blood sugar levels within the target range is essential for reducing the risk of PVD. Regular monitoring, adherence to medication, and following a healthy diet can help manage blood sugar and prevent the progression of atherosclerosis.
- Regular Exercise: Engaging in regular physical activity improves circulation and can help reduce symptoms of PVD, such as claudication. Walking, in particular, is an effective exercise for improving blood flow to the legs.
- Healthy Diet: A heart-healthy diet that is low in saturated fats, cholesterol, and sodium can help manage both diabetes and PVD. Incorporating plenty of fruits, vegetables, whole grains, and lean proteins into your diet supports vascular health and reduces the risk of plaque buildup.
- Quit smoking: Smoking is a major risk factor for PVD and can worsen the effects of diabetes on your blood vessels. Quitting smoking is one of the most important steps you can take to improve your vascular health.
- Medications and Treatment: Your healthcare provider may prescribe medications to help manage PVD and reduce the risk of complications. These may include antiplatelet drugs to prevent blood clots, cholesterol-lowering medications, and medications to improve blood flow. In more severe cases, procedures such as angioplasty or bypass surgery may be necessary to restore blood flow to the affected limbs.
To learn more about how these treatment options can be tailored to your needs, explore our vascular care services that focus on comprehensive and personalized care.
At Risk of Peripheral Vascular Disease?
PVD can progress silently until serious symptoms appear. Early detection and proper care can help preserve mobility and save limbs.

Conclusion
Diabetes significantly increases the risk of developing peripheral vascular disease, making it essential for individuals with diabetes to be proactive about their vascular health. Understanding the connection between diabetes and PVD, recognizing the early signs, and taking steps to manage the condition can help prevent serious complications and improve quality of life.
If you have diabetes and are concerned about your risk of PVD, it is important to work closely with your healthcare provider to develop a personalized plan for managing both conditions. Regular check-ups, lifestyle changes, and appropriate medical treatments are key to maintaining vascular health and reducing the impact of PVD. For more insights into managing diabetes and PVD, visit our comprehensive care approach that prioritizes prevention and long-term well-being.
With the right care and management, individuals with diabetes can significantly reduce their risk of PVD and maintain a healthy, active lifestyle.