Living with diabetes can be challenging, especially when complications like diabetic neuropathy come into play. This condition, affecting nearly half of all individuals with diabetes, can significantly impact quality of life and lead to further issues such as diabetic foot ulcers. Let’s delve into what diabetic neuropathy is, its various forms, and how we can manage and prevent its complications.

What is Diabetic Neuropathy?
Diabetic neuropathy occurs when high blood sugar levels over time cause damage to the nerves. This happens because elevated glucose levels deteriorate the small blood vessels that provide nutrients and oxygen to the nerves. There are three main types of diabetic neuropathy, each affecting different parts of the body and presenting unique challenges.
Sensory Neuropathy
Sensory neuropathy primarily affects the nerves responsible for sensation. If you have this condition, you might experience numbness, tingling, pain, or weakness, particularly in your feet and hands. Unfortunately, the loss of sensation can lead to unnoticed injuries, cuts, or blisters, which can then result in severe infections or ulcers because they go untreated.
Motor Neuropathy
Motor neuropathy impacts the nerves controlling muscle movement. This can lead to muscle weakness, balance issues, and foot deformities like claw toes or hammertoes. These deformities create abnormal pressure points, which can cause calluses and ulcers due to the altered biomechanics of the foot.
Autonomic Neuropathy
Autonomic neuropathy affects the nerves that manage involuntary functions such as heart rate and digestion. It can also impair sweat and oil production, leading to dry, cracked skin. This makes the skin more prone to infections and ulcers due to its compromised integrity.
Diabetic Foot Ulcers: A Dangerous Complication
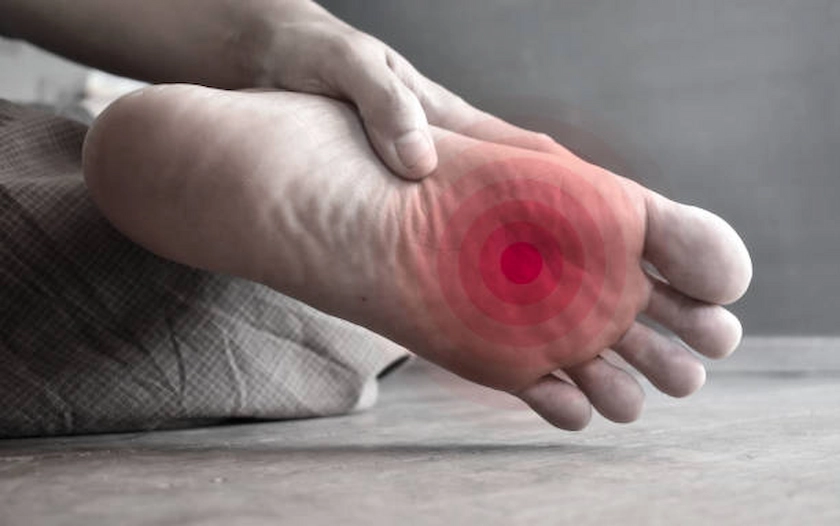
One of the most serious complications of diabetic neuropathy is diabetic foot ulcers. These are open sores that typically appear on the bottom of the foot. They result from a combination of neuropathy, poor circulation, and an inability to heal properly. Foot deformities and inappropriate footwear can also contribute to the formation of these ulcers.
Reduced blood flow, often due to peripheral arterial disease (PAD), is a common issue for diabetics and further complicates healing. Here are some sobering facts about diabetic PAD:
- Approximately 70% of diabetic wounds involve PAD.
- 85% of diabetes-related amputations are preceded by ulcers.
- Two-thirds of older adults undergoing amputation fail to regain independence.
- 70% of individuals who undergo amputation pass away within five years.

Risk Factors for Diabetic Foot Ulcers
The longer you have diabetes, the higher your risk of developing complications like neuropathy and foot ulcers. Chronic high blood sugar levels can damage nerves and blood vessels over time, making foot problems more likely. Poor blood glucose control accelerates this damage, making it harder for your body to heal wounds and easier for ulcers to develop.
Diabetic neuropathy causes a loss of sensation in your feet, making it difficult to notice injuries or pressure points. This can lead to untreated wounds and ulcers. PAD, which reduces blood flow to your extremities, further hampers wound healing and increases the risk of ulcers and infections.
Foot deformities, such as hammertoes, bunions, and Charcot feet, create abnormal pressure points on your feet. These can lead to calluses, blisters, and ulcers due to improper weight distribution. Inappropriate footwear can cause friction and pressure on your feet, leading to blisters, sores, and ulcers.
A history of foot ulcers increases the risk of recurrence because scar tissue from previous ulcers may break down more easily. Poor foot hygiene, such as not washing or inspecting your feet regularly, can result in unnoticed injuries and infections. Smoking impairs circulation and reduces oxygen delivery to tissues, which is crucial for wound healing. It also exacerbates the effects of PAD, further increasing the risk of foot ulcers.
Obesity places additional pressure on your feet, which can cause ulcers. It also contributes to poor blood glucose control and increases the risk of developing diabetes-related complications.
Preventive Measures
To prevent diabetic foot ulcers and other complications, it’s essential to take proactive steps. Regular foot inspections are crucial. Check your feet daily for any abnormalities. Managing your blood glucose levels by keeping your blood sugar within the recommended range helps prevent nerve and blood vessel damage.
Wear appropriate footwear by choosing well-fitting, comfortable shoes that protect your feet. Keep your feet clean and moisturized by washing and drying them daily, and applying moisturizer to maintain skin integrity. Trim your nails carefully, cutting them straight across to avoid injury, and always wear shoes to protect your feet from potential harm.
Stopping smoking improves circulation and oxygen delivery to your tissues. Regular check-ups with a healthcare professional for foot examinations are vital. Exercise regularly to enhance circulation and blood sugar control. Educating yourself about foot care and risk prevention is key to managing your health effectively.
Conclusion
Diabetic neuropathy and its complications, such as foot ulcers, are significant concerns for individuals with diabetes. Understanding and managing these risks through regular care, appropriate footwear, and maintaining blood glucose levels is essential to preventing severe outcomes. Early intervention and consistent management are key to preventing the severe consequences of diabetic neuropathy.
For more personalized advice and treatment, visit Dr. Darryl Lim’s clinic. We’re here to help you take the best possible care of your health.

















