Diabetic foot ulcers are a common and serious complication for individuals living with diabetes. These open sores or wounds often develop on the bottom of the foot and can worsen or become infected if not treated early. Recognizing and addressing an early stage diabetic foot ulcer is key to preventing further complications and maintaining overall foot health. At our clinic in Singapore, we focus on diagnosing and treating diabetic foot ulcers, emphasizing early intervention to help patients stay ahead of potential risks.

What Are Diabetes Foot Ulcers?
Diabetic foot ulcers are open wounds caused by diabetes-related factors like poor circulation, nerve damage, and elevated blood sugar levels. They often result from minor injuries, pressure points, or friction from ill-fitting shoes. Many diabetic patients experience reduced sensation in their feet, which means even small injuries can go unnoticed and progress into ulcers.
If untreated, foot ulcers can lead to serious infections that might require extensive treatment—or, in severe cases, limb amputation. That’s why addressing an early stage diabetic foot ulcer promptly is so important.
Common Causes of Diabetes Foot Ulcers
Understanding the causes of diabetic foot ulcers helps in taking preventive steps. These ulcers are typically triggered by:
- Peripheral Neuropathy: Nerve damage reduces sensation, making it harder to notice cuts, blisters, or other injuries.
- Poor Circulation: Diabetes can impair blood flow, slowing down the healing process.
- High Blood Sugar Levels: Elevated glucose weakens the immune system, increasing the risk of infections.
- Foot Deformities: Conditions like bunions or calluses can create pressure points that lead to ulcers.
- Inappropriate Footwear: Ill-fitting shoes can rub against the skin, causing blisters that may develop into ulcers.
Taking steps to address these risks can go a long way in protecting foot health.
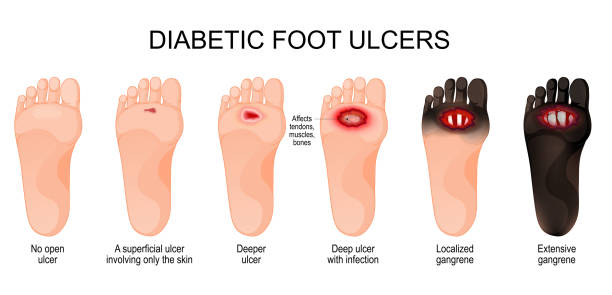
Recognizing Early Stage Diabetic Foot Ulcers
Spotting an early stage diabetic foot ulcer can prevent complications down the road. Keep an eye out for:
- Redness or Swelling: Inflammation or unhealed injuries can signal the start of an ulcer.
- Blisters or Calluses: These can worsen into ulcers if not cared for properly.
- Drainage on Socks or Shoes: Fluid leaking from a wound may indicate a developing ulcer.
- Discoloration or Dark Spots: These can signal poor blood flow and should be evaluated immediately.
If you notice any of these signs, it’s time to seek medical attention. Early diagnosis and treatment can significantly reduce the risk of severe complications.
Treatment Options for Early Stage Diabetic Foot Ulcers
When it comes to treating diabetic foot ulcers, early intervention is crucial. Treatment options typically include:
- Wound Care: Cleaning the ulcer, applying sterile dressings, and using advanced wound care products to promote healing.
- Debridement: Removing dead or damaged tissue to encourage healing and reduce infection risk.
- Antibiotic Therapy: If an infection is present, antibiotics may be prescribed to stop it from spreading.
- Offloading: Relieving pressure on the ulcer using specialized shoes, casts, or crutches to support faster healing.
- Moisture Control: Maintaining the right moisture balance around the wound with advanced dressings to create an ideal healing environment.
- Optimization of Blood Supply: If poor blood circulation is found to be affecting wound healing, keyhole procedures like angioplasty or stenting can improve blood supply to the area, enhancing the body’s natural healing processes.
Each treatment plan is tailored to the ulcer’s severity and location to provide effective and lasting relief.
Preventing diabetic foot ulcers
Prevention is always better than cure. Diabetic patients can take simple steps to reduce the likelihood of developing foot ulcers:
- Inspect Feet Daily: Look for cuts, blisters, or colour changes and address them early.
- Moisturise Regularly: Keep your skin soft, but avoid applying lotion between the toes to prevent fungal infections.
- Wear Comfortable Footwear: Ensure shoes fit well and reduce pressure points.
- Trim Nails Properly: Cut toenails straight across to avoid ingrown nails and infections.
- Manage Blood Sugar Levels: Controlling glucose levels reduces the risk of neuropathy and poor circulation.
These daily habits can significantly lower the risk of complications and improve long-term foot health.
The Role of Regular Check-Ups in Diabetic Foot Health
Routine check-ups are vital for spotting and managing early-stage diabetic foot ulcers. A thorough evaluation helps detect ulcers, neuropathy, and circulation issues before they worsen.
Regular visits also provide an opportunity for patients to ask questions, receive updated guidance on foot care, and make any necessary adjustments to their preventive routines. It is essential that patients stay proactive about their foot health, especially in Singapore’s warm, humid climate where foot infections can become more common.
Dealing with Diabetic Foot Problems?
Diabetes can lead to serious foot complications if not addressed early. Get expert care to protect your feet and prevent further issues.

Conclusion
Recognising and treating an early stage diabetic foot ulcer is essential for managing diabetes and avoiding serious complications. Dr. Darryl Lim and team specialize in early intervention and personalized care to help patients maintain healthy feet and overall well-being.
If you’re experiencing signs of a foot ulcer or want guidance on diabetic foot care, consider scheduling a consultation today. Taking proactive steps now can make all the difference in protecting your foot health.

















