Gangrene is a serious condition where body tissue dies due to poor blood flow or an infection. For diabetics, the toes and feet are especially at risk because of reduced circulation and nerve damage. Recognizing the signs and symptoms of toe gangrene early is critical—timely treatment can prevent the condition from worsening. Dr. Darryl Lim is a Vascular Specialist in Singapore, who specializes in managing diabetic foot complications, including gangrene, to help protect foot health and prevent serious outcomes.
What Is Toe Gangrene?
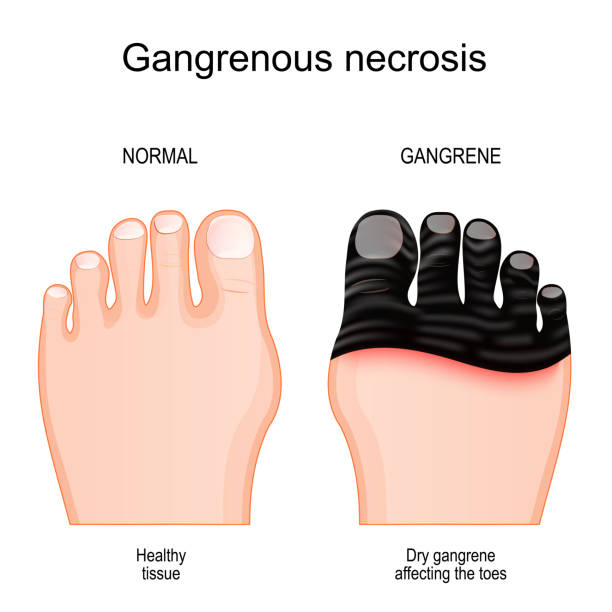
Gangrene in the toe happens when blood flow is cut off, leading to tissue death. There are two main types:
- Dry Gangrene: Caused by poor circulation, it appears as dry, shriveled, and discolored skin.
- Wet Gangrene: This develops from an infection, with symptoms like swelling, blistering, and a foul smell.
Both types are serious and need immediate medical attention. For diabetics, reduced sensation in the feet can make it harder to notice early warning signs, which is why regular foot checks are so important.

Spotting Gangrene Toe Symptoms Early
Spotting the symptoms early can make all the difference. Here’s what to look out for:
- Discoloration: Toes may turn black, blue, green, or pale white, either in patches or across the entire toe.
- Pain or Numbness: Intense pain might be followed by numbness as the tissue begins to die.
- Cold, Shriveled Skin (Dry Gangrene): Skin might feel cold and appear dry or shriveled.
- Swelling and Blisters (Wet Gangrene): This type often causes fluid-filled blisters and foul-smelling discharge.
- Loss of Sensation: Neuropathy can mask pain, allowing gangrene to progress unnoticed.
If you notice any of these gangrene toe symptoms, don’t ignore them. Early medical attention can significantly improve outcomes.
Risk Factors for Toe Gangrene in Diabetic Patients
Certain factors increase the risk of gangrene in patients with diabetes:
- Peripheral Artery Disease (PAD): Reduced blood flow to the extremities slows wound healing, increasing the risk of complications.
- Diabetic Neuropathy: Nerve damage in the feet can mask injuries, allowing them to worsen unnoticed.
- High Blood Sugar Levels: Poorly controlled glucose can weaken the immune system and make infections harder to fight.
- Foot Deformities or Pressure Points: Bunions, calluses, or other foot conditions can create pressure points that lead to injuries.
Understanding these risks helps patients take proactive steps to protect their foot health.

Treatment Options for Toe Gangrene
When gangrene is detected, acting quickly is vital to stop it from progressing and to save as much tissue as possible. Treatment options include:
- Antibiotics:
If an infection is present, antibiotics (oral or intravenous) are often the first step to control and prevent the spread of bacteria. - Debridement:
This involves removing dead or infected tissue to promote healing and lower the risk of further complications. The procedure is carefully performed to preserve as much healthy tissue as possible. - Optimising Blood Flow (Angioplasty and Stenting):
Keyhole procedures like angioplasty can help restore proper blood flow, delivering oxygen and nutrients to the affected area. Improved circulation can significantly enhance the healing of existing wounds. - Hyperbaric Oxygen Therapy (HBOT):
In some cases, HBOT can be beneficial. This treatment involves breathing pure oxygen in a pressurised chamber, which increases blood oxygen levels, promotes healing, and helps fight infection. - Amputation (as a Last Resort):
If gangrene is too advanced or poses a risk of spreading infection, amputation of the affected toe may be necessary to protect the patient’s overall health.
Dr. Lim prioritizes limb-preserving treatments and only considers amputation as a last resort. Our goal is to preserve healthy tissue and maintain function whenever possible.
Preventing Gangrene in Diabetic Patients
Prevention is key for diabetic patients. Here are some practical steps:
- Inspect Your Feet Daily: Look for any cuts, blisters, or changes in colour.
- Practice Good Foot Hygiene: Wash and dry your feet daily, and moisturise to keep the skin soft—avoiding lotion between the toes.
- Wear Proper Footwear: Ensure shoes fit well and provide support to reduce pressure points.
- Control Blood Sugar Levels: Stable glucose levels help maintain good circulation and reduce infection risk.
- Seek Immediate Treatment for Injuries: Even minor wounds should be evaluated if they don’t heal quickly.
Taking these steps can reduce the risk of complications like gangrene and help protect long-term foot health.
Dealing with Diabetic Foot Problems?
Diabetes can lead to serious foot complications if not addressed early. Get expert care to protect your feet and prevent further issues.

Conclusion
Recognizing the symptoms of toe gangrene early and seeking help can significantly improve treatment outcomes. At Dr. Darryl Lim’s clinic, we’re dedicated to providing personalized care for diabetic foot complications, including gangrene.
If you’re concerned about your foot health, don’t wait—schedule a consultation today. Early intervention can save tissue, prevent complications, and help you stay one step ahead of serious conditions.

















