Venous leg ulcers are a significant and often frustrating medical condition, primarily affecting the lower parts of the legs. They result from chronic venous insufficiency (CVI), a condition where the veins in your legs struggle to pump blood back to the heart efficiently. This inefficiency leads to prolonged wound healing and considerable discomfort.
Understanding the Causes
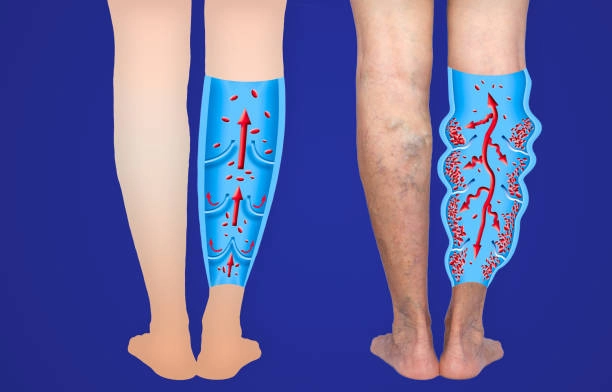
Several factors can contribute to the development of venous leg ulcers. Chronic venous insufficiency is the most common culprit. When your leg veins can’t efficiently return blood to the heart, pressure builds up, causing fluid to leak into surrounding tissues. This fluid buildup can lead to skin breakdown and ulcer formation. Often, CVI also causes varicose veins, those twisted and enlarged veins that are not just a cosmetic concern but a sign of deeper venous issues.
Another significant factor is deep vein thrombosis (DVT), where blood clots in the deep veins of the legs increase venous pressure and damage the valves in the veins. Obesity can exacerbate these issues by adding extra pressure on your leg veins, while prolonged standing or sitting can impair blood flow, further increasing venous pressure. Previous leg injuries or surgeries, as well as the natural aging process, also contribute to the risk by weakening the veins and affecting circulation.
Recognizing the Symptoms
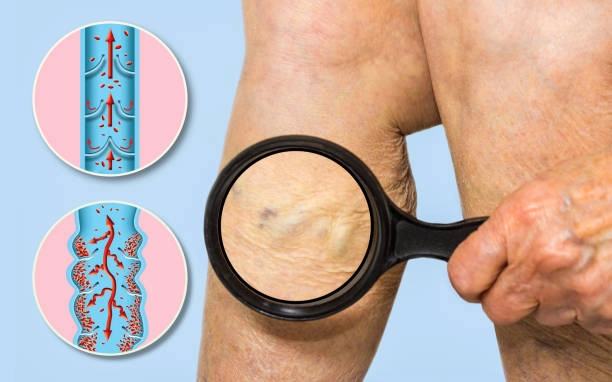
Identifying venous leg ulcers early can make a significant difference in treatment outcomes. Typically, these ulcers present as open sores on the inner side of the lower leg, just above the ankle. You might notice reddish-brown skin changes around the ulcer, a condition known as hemosiderin staining. Swelling, especially after long periods of standing, is another common symptom. The area around the ulcer might itch or burn due to inflammation, and the pain can range from mild to severe. The skin around the ulcer often hardens and becomes tender, a condition called lipodermatosclerosis. If the ulcer is infected, it might drain fluid that can be either clear or purulent.
Diagnosing Venous Leg Ulcers
Diagnosing venous leg ulcers typically involves a thorough clinical evaluation. Your doctor will review your symptoms, risk factors, and medical history before conducting a detailed physical examination of the ulcer and surrounding skin. Diagnostic tests such as a Doppler ultrasound may be used to assess blood flow and check for abnormalities in the veins, such as venous reflux or deep venous thrombosis. In some cases, an ankle-brachial index (ABI) measurement might be necessary to rule out concomitant arterial disease. Venography, an imaging test, can help visualize the veins if the ultrasound results are inconclusive. Blood tests are often conducted to detect underlying conditions like diabetes or infections that might be complicating the ulcer.
Treatment Options
Managing venous leg ulcers effectively requires a multi-faceted approach. Compression therapy is fundamental, involving the use of compression bandages or stockings to improve venous return and reduce swelling. Proper wound care is also crucial. This includes regularly cleaning the ulcer, removing dead tissue through debridement, and applying suitable dressings to keep the wound moist and promote healing.
Medications play a vital role as well. Topical agents, such as antiseptics or antibiotics, are used if there’s an infection, while systemic antibiotics might be necessary for more severe infections. In some cases, surgical interventions can be beneficial. Procedures like endovenous vein ablation address the underlying venous insufficiency, while surgical debridement removes necrotic tissue to promote healing.
Prevention Strategies
Preventing venous leg ulcers or their recurrence involves several proactive steps. Regular exercise, such as walking or swimming, can significantly improve calf muscle function and venous return. Maintaining a healthy weight reduces the pressure on your leg veins. It’s also important to avoid prolonged periods of standing or sitting. If your job requires long periods of immobility, try to move around regularly to encourage blood flow.
Wearing compression stockings can help maintain proper blood flow, and choosing comfortable, supportive footwear can prevent unnecessary pressure on your legs. Adopting a healthy diet supports overall vascular health, and regular check-ups with your healthcare provider can help catch any issues early. Additionally, learning proper foot and leg care is essential in managing your vein health.
Conclusion
Venous leg ulcers are a serious and often debilitating condition that requires comprehensive treatment and prevention strategies. By understanding the causes, recognizing the symptoms early, and adhering to preventive measures, you can significantly reduce your risk of developing these ulcers. At Dr. Darryl Lim’s clinic, we are committed to providing personalized advice and treatment to help you manage your vein health and improve your quality of life. For more detailed information, explore our resources and services for managing venous conditions.