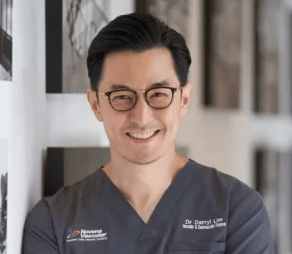
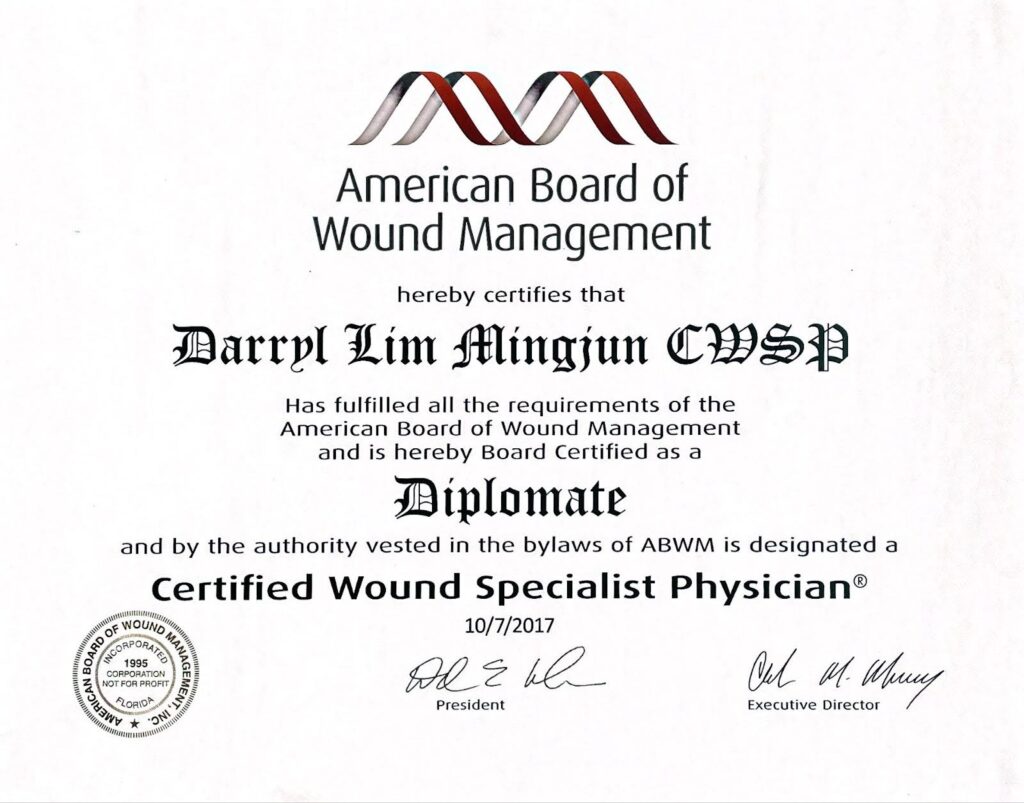
Wounds and cuts are common, but for diabetic patients, the difference between a healing and a non-healing wound can have serious implications. While most wounds close and heal naturally, non-healing wounds remain open, often becoming vulnerable to infection. Understanding what affects wound healing, especially for those managing diabetes, is essential to prevent complications. Dr. Darryl Lim, a Certified Wound Specialist Physician (CWSP) by the American Board of Wound Management, has a special interest in managing diabetic foot ulcers. He focuses on advanced treatment methods to promote healing and prevent long-term complications.
What defines a non-healing wound?
A non-healing wound, sometimes called a chronic wound, is one that fails to close within an expected period—typically around four weeks. Diabetic patients are particularly susceptible to non-healing wounds due to factors like reduced blood circulation, nerve damage, and a weakened immune response, all of which can slow the natural healing process. Without proper care, these wounds can lead to infections, tissue damage, or even amputation in severe cases.

How to tell if a wound is healing properly
Identifying the differences between healing and non-healing wounds can guide how to approach wound care. Key distinctions include:
- Wound Edges: A healing wound usually has pink edges that gradually close, signaling tissue growth. In contrast, non-healing wounds often have dark, swollen, or uneven edges with little to no progress in closure.
- Signs of Infection: Healing wounds generally stay clean, while non-healing wounds may show redness, swelling, or pus, indicating infection.
- Pain Levels: Tenderness is common initially for healing wounds, but pain typically decreases as healing progresses. With non-healing wounds, pain may persist or even worsen due to infection or tissue damage.
- Discharge: A healing wound may have minimal discharge as part of the healing process. However, continuous or foul-smelling discharge from a wound can signal infection in a non-healing wound.
- Skin Discoloration: Healthy or pinkish skin often surrounds a healing wound, while darkened or discolored skin near a wound may suggest poor circulation, a common trait in non-healing wounds.
If you notice any of these symptoms, it’s essential to seek medical attention right away. Dr. Darryl Lim offers careful assessments to diagnose and manage non-healing wounds, with a focus on preventing complications and supporting healing.
Common reasons for non-healing wounds in diabetic individuals
Several underlying factors contribute to why people with diabetes experience non-healing wounds more frequently:
- Poor Circulation: Diabetes can impair blood vessels, reducing the flow of oxygen and nutrients needed for healing, especially in extremities.
- Diabetic Neuropathy: Nerve damage in the feet can diminish sensation, making it difficult to detect injuries. Unnoticed minor wounds can worsen over time without proper care.
- Elevated Blood Sugar Levels: High blood glucose weakens the body’s ability to fight infection and increases inflammation, slowing down healing.
- Compromised Immune System: Diabetes can weaken immune response, making it harder for the body to repair tissue and fight infections.
These factors require that individuals with diabetes take extra steps to prevent wounds from progressing to a chronic, non-healing state.

Advanced treatment options for non-healing wounds
Addressing recalcitrant wounds often involves specialized techniques that go beyond standard wound care. Dr. Lim provides a range of advanced treatment options for managing such wounds:
- Wound Cleaning and Dressing: Regular wound cleaning and dressing are essential to prevent infection and create a healing environment. This involves sterile dressings and keeping the wound moist to aid recovery.
- Debridement: Removing dead or infected tissue from the wound area stimulates healthy tissue growth and prevents further infection. This procedure focuses on removing only the affected tissue to aid healing.
- Antibiotic Therapy: When a wound is infected, antibiotics can help control bacterial growth and prevent the infection from spreading.
- Pressure Offloading: Reducing pressure on the wound, particularly on weight-bearing areas, allows healing to proceed. Specialized footwear, orthotic devices, or casts may be recommended to relieve pressure on foot wounds.
- Vacuum-Assisted Dressings (VAC): VAC dressings use negative pressure to remove excess fluid, reduce swelling, and promote the formation of healthy tissue. This creates an optimal environment for wound healing and is particularly effective for deep or complex wounds.
- Electrical Stimulation (ES): ES therapy applies low-level electrical currents to the wound, which can encourage tissue regeneration, increase blood flow, and reduce bacterial load.
- Angioplasty and Stenting: Blood supply to non-healing diabetic wounds is often reduced due to peripheral vascular disease. In such cases, angioplasty and stenting can help restore blood flow to the area, supporting the healing process.
Each treatment plan is tailored to the patient’s specific needs, combining approaches to achieve optimal healing and prevent recurrence.
Steps to prevent non-healing wounds
Prevention plays a crucial role in avoiding non-healing wounds, especially for those managing diabetes. Incorporating the following habits into daily routines can help maintain foot health and reduce the likelihood of wounds becoming chronic:
- Inspect Feet Daily: Regularly check for any cuts, blisters, or color changes. Early detection and treatment of minor injuries can prevent complications.
- Maintain Proper Foot Hygiene (Keep Feet Clean and moisturized): Wash and dry feet thoroughly each day, and apply moisturizer to prevent dry or cracked skin. Avoid putting excessive lotion between the toes to prevent fungal infections.
- Trim Toenails Carefully: Trim nails straight across to avoid ingrown toenails, which can easily get infected if left untreated.
- Choose Protective Footwear: Properly fitted shoes help avoid pressure points that can lead to injuries. Diabetic-friendly footwear adds extra support to minimize risks.
- Control Blood Sugar Levels: Stable blood glucose levels lower the risk of neuropathy and circulation problems, both of which contribute to non-healing wounds.
- Seek Prompt Treatment for Minor Injuries: Address even small cuts or blisters as soon as possible, especially if they don’t heal within a few days.
Following these preventive measures can help reduce the risk of developing non-healing wounds.
Why non-healing wounds need specialized care
Non-healing wounds need specialized care, particularly for diabetic patients, because of the unique challenges that come with diabetes like poor blood circulation and nerve damage. Managing these complex wounds often requires more than standard treatment. General practitioners may not have the resources or expertise to manage these complex wounds, so specialized care is often necessary to ensure that non-healing wounds receive the attention they need. Dr. Darryl Lim provides advanced treatments for wound care, focusing on personalized care to support healing and prevent complications.
When to seek medical help for a wound that isn’t healing
It’s crucial for diabetic patients to monitor their wounds closely and seek medical care if:
- An open sore or wound hasn’t shown improvement within a few days
- There is pain, swelling, or foul-smelling discharge from the wound
- The skin around the wound darkens or becomes discolored
- Numbness or reduced sensation develops in the affected area
Seeking help early is essential to prevent the wound from worsening and to encourage healing. Our clinic provides thorough foot assessments and customized treatment plans to manage non-healing ulcers effectively.
Conclusion
For individuals with diabetes, distinguishing between healing and non-healing wounds is crucial. Untreated non-healing wounds can lead to significant complications, but with early intervention and the right treatment approach, effective healing is possible.
In Singapore, Dr. Darryl Lim is one of a handful of Certified Wound Specialist Physicians (CWSP) qualified to provide specialized diabetic foot care, helping patients work toward lasting foot health. If you’re dealing with a non-healing ulcer or need guidance on diabetic foot care, consider scheduling a consultation. Early treatment is key to achieving the best outcomes and prevent further complications.