Ingrown toenails, or onychocryptosis, happen when the edges of your toenail grow into the surrounding skin, causing pain, redness, and swelling. This can be particularly worrisome for people with diabetes due to their increased risk of infection and slower healing rates. Let’s dive into what causes ingrown toenails, how to prevent them, and what to do if you get one.

Causes of Ingrown Toenails
Understanding what causes ingrown toenails can help you avoid them. One common cause is improper trimming. If you cut your toenails too short or don’t cut them straight across, the nail can grow into the skin. Wearing tight shoes that squeeze your toes can also push the nail into the surrounding skin. Injuries to the toenail, such as stubbing your toe, can change how your nail grows. Genetics can play a role too, as some people naturally have curved or thick toenails that are more prone to becoming ingrown. Lastly, poor foot hygiene and fungal infections can thicken or deform your toenails, increasing the risk of ingrown toenails.
Risks for Diabetics
People with diabetes need to be extra careful because they face higher risks when it comes to ingrown toenails. Poor blood circulation slows down wound healing, and nerve damage can reduce pain sensation, making it easy to miss an injury. Foot deformities, which are more common in diabetics, can also increase pressure on the toes, leading to ingrown toenails.

Symptoms to Watch For
If you have an ingrown toenail, you might notice redness and swelling around the nail, pain or tenderness in the affected toe, and possibly pus or fluid discharge if there’s an infection. A foul smell from the infected area can also be a sign that something’s wrong.
Severity Grading
Ingrown toenails can range from mild to severe. In mild cases, you might see redness, swelling, and pain. As it progresses to moderate, you might notice increased swelling, pain, and discharge. Severe cases involve the overgrowth of granulation tissue and possible abscess formation.
Preventive Measures
To prevent ingrown toenails, proper nail trimming is essential. Cut your nails straight across without rounding the corners to avoid the nail growing into the skin. Make sure your shoes fit well and provide plenty of room for your toes. Regular foot checks, especially for diabetics, can catch early signs of problems.
Conservative Management
For mild cases, you can try elevating the nail using cotton, dental floss, or a gutter splint to relieve pressure. Applying topical antibiotics and antiseptics can prevent infection. Pain relief can be managed with NSAIDs or paracetamol to reduce pain and inflammation.
When to See a Doctor
If you have diabetes or if your ingrown toenail doesn’t improve with home treatment, it’s important to see a doctor. This is crucial to prevent severe complications like gangrene. Professional management might include assessing circulation before any surgical intervention due to diabetes-related circulation issues.
Professional Management and Treatment
When conservative methods don’t work, or if the ingrown toenail is severe, medical intervention might be necessary. Treatments can include partial nail avulsion with phenol matricectomy to remove part of the nail and prevent regrowth, wedge resection with surgical matricectomy (Zadik’s Procedure) for severe cases, and complete nail avulsion with matrixectomy for extensive problems. Severe infections may require debridement and drainage, followed by antibiotics to control the infection.
Post-Surgical Care
After surgery, keeping the wound clean and dry is crucial. Follow your doctor’s instructions for dressing changes, and attend regular follow-up appointments to monitor healing and prevent recurrence. Maintaining good foot hygiene, wearing proper footwear, and avoiding trauma to the toes are important steps in your recovery.
Conclusion
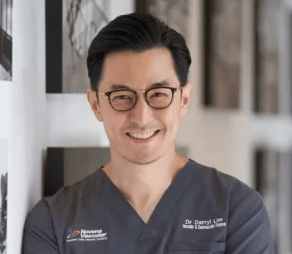
Dr. Lim works closely with an in-house podiatrist to ensure thorough and holistic care for patients with ingrown toenails. Managing ingrown toenails effectively is particularly important for individuals with diabetes. Regular inspections, preventive measures, and prompt treatment are essential to avoid complications. For personalized advice and treatment, visit Dr. Darryl Lim’s clinic in Singapore. Our expert team is dedicated to providing comprehensive care for all your foot health needs.