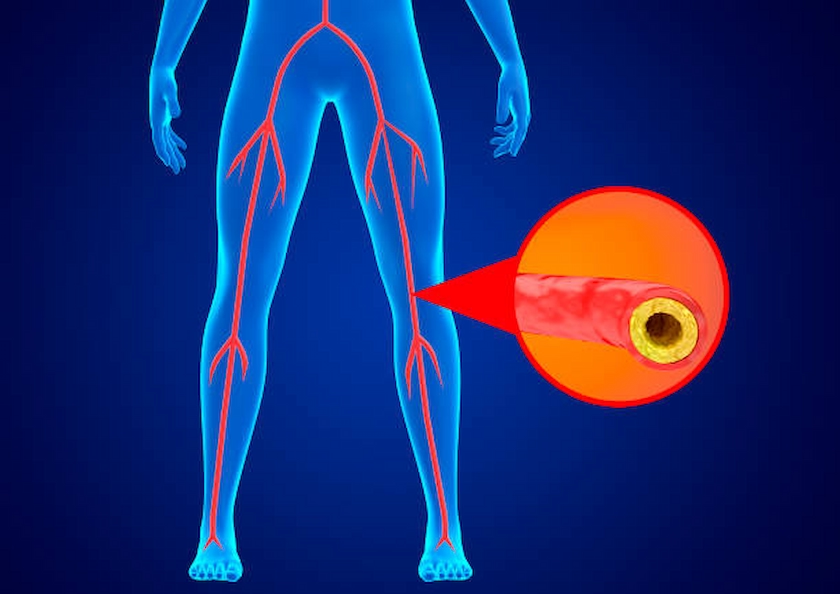
Peripheral Vascular Disease (PVD) is a common yet often misunderstood condition that affects millions of people worldwide. It occurs when the arteries that supply blood to your limbs, particularly the legs, become narrowed or blocked due to the buildup of fatty deposits, known as plaque. This condition can lead to significant discomfort, reduced mobility, and even serious health complications if left untreated. Understanding the key facts about PVD is essential for recognizing the signs, seeking appropriate treatment, and managing the condition effectively.
PVD is Caused by Atherosclerosis
The primary cause of peripheral vascular disease is atherosclerosis, a condition in which plaque builds up on the walls of the arteries. Over time, this plaque hardens and narrows the arteries, reducing blood flow to the limbs. While atherosclerosis can affect any artery in the body, when it occurs in the arteries of the legs or arms, it leads to PVD. The reduced blood flow caused by PVD can result in symptoms such as leg pain, cramping, and fatigue, particularly during physical activity.
PVD is often undiagnosed
Many people with PVD do not experience symptoms in the early stages, or they may mistake their symptoms for other conditions, such as arthritis or simply getting older. As a result, PVD often goes undiagnosed until it reaches a more advanced stage. Regular screenings and check-ups are crucial, especially for individuals with risk factors like smoking, diabetes, high blood pressure, or high cholesterol. Early diagnosis can lead to better outcomes and prevent complications.
Leg pain is a common symptom.
One of the hallmark symptoms of PVD is leg pain or cramping, known as claudication. This pain typically occurs in the muscles of the calves, thighs, or buttocks during activities like walking or climbing stairs. The pain usually subsides with rest, only to return when physical activity resumes. Claudication occurs because the muscles are not receiving enough oxygen-rich blood due to the narrowed arteries. As PVD progresses, this pain may occur more frequently and even at rest.
PVD increases the risk of heart attack and stroke.
PVD is more than just a problem with the arteries in your legs. It is a systemic condition that indicates widespread atherosclerosis, which can also affect the arteries supplying the heart and brain. This means that individuals with PVD are at a significantly higher risk of having a heart attack or stroke. In fact, PVD often indicates more widespread cardiovascular disease. Managing PVD effectively involves addressing overall cardiovascular health to reduce these risks.
Lifestyle Changes Can Make a Big Difference
One of the most effective ways to manage PVD and reduce symptoms is through lifestyle changes. Quitting smoking is the single most important step, as smoking is a major risk factor for PVD and accelerates the progression of atherosclerosis. Regular exercise, such as walking, can improve circulation and help alleviate symptoms of claudication. A hearty diet that is low in saturated fats, cholesterol, and sodium can also help manage PVD and its associated risks.
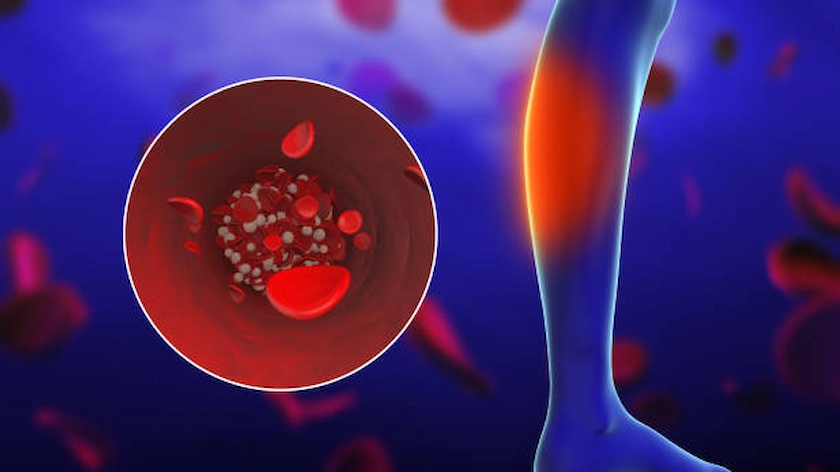
Medications and Treatments Are Available
In addition to lifestyle changes, there are several medical treatments available for PVD. These may include medications to manage symptoms, improve blood flow, and reduce the risk of blood clots. For more advanced cases, minimally invasive procedures like angioplasty or stenting may be necessary to open up narrowed arteries. In severe cases, surgical options such as bypass surgery may be required to restore adequate blood flow to the affected limb. Working with a healthcare provider to develop a personalized treatment plan is essential for managing PVD effectively.
PVD Can Lead to Serious Complications if Left Untreated
If PVD is not diagnosed and treated, it can lead to serious complications, including critical limb ischemia (CLI), a severe form of PVD. CLI occurs when the blood flow to the limbs is so restricted that it causes persistent pain, non-healing sores, and even tissue death (gangrene). In severe cases, this can lead to amputation. Additionally, the increased risk of heart attack and stroke associated with PVD underscores the importance of early detection and management.
Regular Check-Ups Are Essential
Given the silent nature of PVD in its early stages and the serious risks it poses, regular check-ups with your healthcare provider are crucial. This is especially true for individuals with risk factors such as smoking, diabetes, or a family history of cardiovascular disease. Simple, non-invasive tests like the ankle-brachial index (ABI) can help detect PVD early, allowing for timely intervention and better outcomes.
For more detailed information on how we approach the diagnosis and management of PVD, explore our comprehensive vascular care services designed to meet the unique needs of each patient.
At Risk of Peripheral Vascular Disease?
PVD can progress silently until serious symptoms appear. Early detection and proper care can help preserve mobility and save limbs.
Conclusion
Peripheral Vascular Disease is a serious condition that requires attention and care. Understanding the key facts about PVD can help you recognize the symptoms, seek appropriate medical advice, and take steps to manage the condition effectively. By making lifestyle changes, working closely with your healthcare provider, and staying informed about your vascular health, you can reduce the risk of complications and improve your overall quality of life.
If you suspect you might have PVD or are at risk, it’s important to take action early. Regular screenings and proactive management are key to maintaining vascular health and preventing the severe consequences of this condition. To learn more about how we can support your vascular health, visit our vascular treatment page for insights and resources.
Your vascular health is integral to your overall well-being, and with the right care, you can manage PVD and lead a healthy, active life.