Pelvic Congestion Syndrome: What Every Woman Should Know (Part 1- Symptoms and Diagnosis)
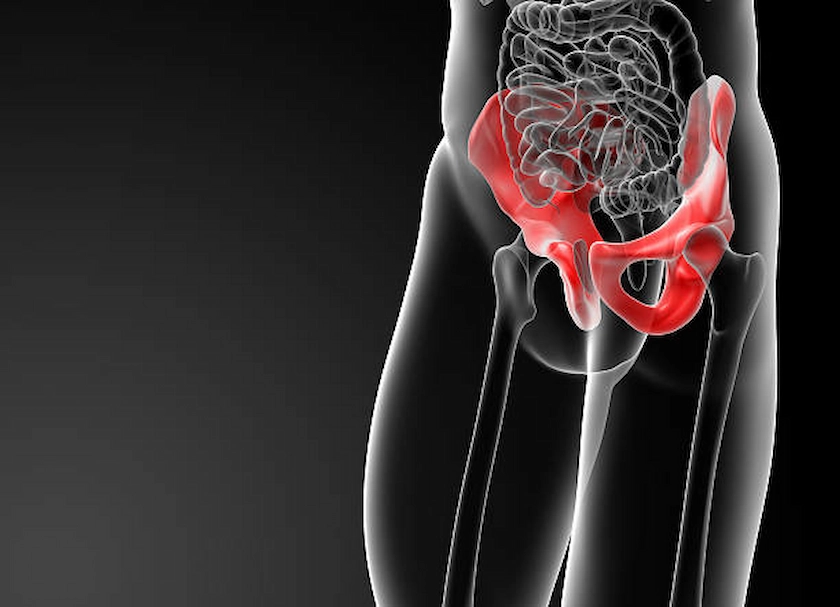
Pelvic Congestion Syndrome (PCS) is an underdiagnosed yet significant cause of chronic pelvic pain in women, especially those of childbearing age. Often mistaken for other gynecological conditions, PCS involves dilated pelvic veins and symptoms like a dull, persistent ache that worsens with standing or after intercourse. This first part of our series explores the symptoms, causes, risk factors, and diagnostic methods used to uncover this hidden condition.