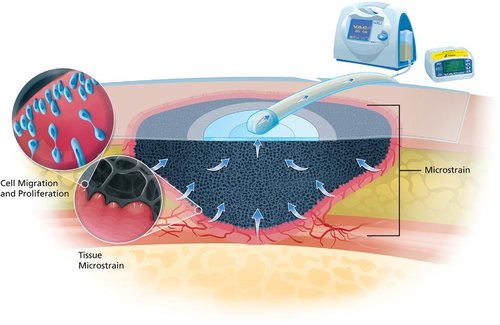
When dealing with a stubborn wound that just won’t heal, traditional bandages might not always do the trick. This is where VAC dressings come into play. VAC stands for Vacuum-Assisted Closure, a specialized wound dressing system designed to promote faster and more effective healing. Unlike regular dressings, a VAC dressing uses controlled negative pressure (suction) to remove excess fluid and reduce swelling around the wound, creating an optimal environment for your body to repair itself.

How VAC Dressings Work
A VAC dressing uses gentle suction to help wounds heal faster. A foam dressing is placed directly over the wound and sealed all around with an airtight film. A small pump then creates negative pressure, drawing out excess fluid, bacteria, and debris. This not only cleans the wound but also boosts blood flow, encouraging the growth of new, healthy tissue.
Benefits of Using VAC Dressings
VAC dressings offer several advantages over traditional wound care methods:
- Accelerated Healing: By continuously removing excess fluid and reducing swelling, VAC dressings can speed up the healing process, helping wounds close more quickly.
- Reduced Infection Risk: The removal of fluid and debris lowers the chances of bacterial growth, thereby reducing the risk of infection.
- Enhanced Tissue Regeneration: Increased blood flow brings more oxygen and nutrients to the wound site, fostering the growth of new tissue.
- Pain Management: Many patients find that VAC dressings help alleviate pain by reducing pressure around the wound.
- Versatility: VAC dressings are effective for a wide range of wounds, including surgical incisions, traumatic injuries, diabetic ulcers, and pressure sores.
Who Can Benefit from VAC Dressings?
VAC dressings are suitable for individuals facing various types of wounds that are slow to heal or prone to complications. Common candidates include:
- Surgical Patients: After major surgeries, a modified version of the VAC dressing (3M™ Prevena™ can help prevent infection and promote faster healing of surgical incisions.
- Diabetic Ulcers: For those with diabetes, wounds on the feet or legs can be particularly stubborn. VAC dressings can enhance healing and reduce the risk of severe complications.
- Traumatic Injuries: Accidents that cause deep or extensive wounds can benefit from the enhanced cleaning and healing environment provided by VAC dressings.
- Pressure Sores: Individuals who are bedridden or have limited mobility may develop pressure sores, which VAC dressings can help manage and heal effectively.
The Procedure: Getting Started with VAC Dressing
Starting with a VAC dressing involves a few straightforward steps, usually performed by a healthcare professional:
- Preparation: The wound is thoroughly cleaned to remove any debris or bacteria.
- Dressing Application: A foam or gauze dressing is cut to fit the wound and placed directly over it.
- Sealing: An airtight film is applied over the dressing to create a sealed environment.
- Connecting the Pump: Tubing is attached to the dressing, leading to the vacuum pump. The pump is then turned on to begin the negative pressure therapy.
- Monitoring: The dressing and pump are regularly monitored and maintained to ensure the system is functioning correctly.
Living with a VAC Dressing
Adjusting to life with a VAC dressing is generally manageable, thanks to modern, portable systems designed for patient comfort and mobility. Here are a few tips to help you adapt:
- Stay Active: Depending on the wound’s location and severity, you may be able to move around and continue daily activities. Always follow your healthcare provider’s advice regarding physical activity.
- Maintain Hygiene: Keep the dressing and surrounding skin clean to prevent infections. Your medical team will guide you on how to care for the dressing at home.
- Regular Check-Ins: Schedule follow-up appointments with your healthcare provider to monitor the wound’s progress and adjust the treatment as needed.
- Manage the Device: Learn how to operate the VAC pump properly and know what to do if you encounter any issues with the system.
Potential Risks and Considerations
While VAC dressings are highly effective, it’s important to be aware of potential risks:
- Infection: Although VAC dressings reduce infection risk, improper handling or a compromised seal can introduce bacteria.
- Skin Irritation: The adhesive film can sometimes cause irritation or allergic reactions in sensitive individuals.
- Bleeding: Excessive suction may lead to bleeding, especially in highly vascularized wounds.
- Device Malfunctions: Problems with the pump or tubing can interrupt the therapy, so it’s crucial to report any issues to your healthcare provider promptly.
Choosing the Right Wound Care Specialist
Selecting a knowledgeable and experienced wound care specialist is key to successful VAC dressing therapy. A wound specialist can assess your wound, determine if VAC dressing is the right option, and guide you through the treatment process. They will also help you navigate any challenges that arise, ensuring you receive the best possible care tailored to your specific needs.
Poorly Healing Wound?
Chronic wounds can be frustrating and slow to heal. Advanced therapies are available to speed recovery and reduce the risk of infection.

Moving Forward with Effective Wound Management
VAC dressings are a significant advancement in wound care, helping wounds heal faster and preventing complications. By understanding how they work and their benefits, and by collaborating with a skilled healthcare provider, you can achieve healthier, more comfortable healing.
For expert guidance, consider consulting a certified wound care specialist like Dr. Darryl Lim. As a Certified Wound Specialist Physician (CWSP) by the American Board of Wound Management, Dr. Lim has extensive experience in managing complex wounds. His personalized approach ensures you receive the most effective treatment tailored to your needs, helping you navigate wound healing with better overall health outcomes.

















