Varicose veins don’t usually appear overnight. For many people, the first signs feel more like minor annoyances rather than a clear medical issue. Perhaps there’s a slight heaviness in your legs after standing all day, or you notice thin, twisting veins beneath the skin that you never saw before. At this early point, the veins may not look dramatically different, and you might dismiss the odd ache or mild discomfort as a passing inconvenience. Yet this subtle beginning often marks the first stage of a process that can worsen over time if left unaddressed.
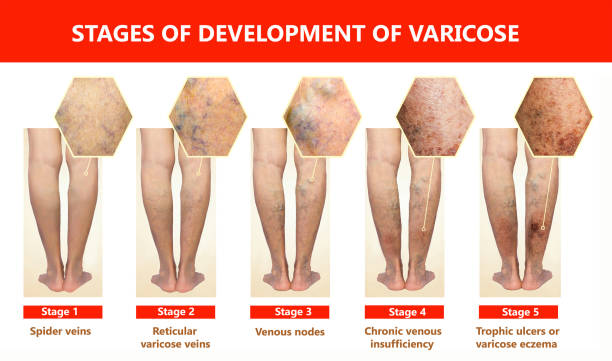
In these initial stages, known informally as “mild varicosities,” the affected veins may appear a bit larger or more pronounced than normal. You might notice them after a hot shower or a long shift on your feet. Though discomfort may be minimal, this early phase is your body’s way of waving a small flag, letting you know that blood isn’t circulating quite as efficiently as it should. While it’s easy to ignore these early warning signs, paying attention now can sometimes prevent more serious issues down the road.
Progressing to Moderate Changes
As varicose veins progress, changes become more visible and harder to dismiss. What began as faint lines under the skin can transform into clearly noticeable twisting or bulging veins. Instead of just a mild heaviness at the end of the day, you might start to feel a dull ache or a sense of fatigue in your legs. Swelling around the ankles might appear if you spend hours sitting in an office chair or standing behind a counter. These moderate varicosities still aren’t typically dangerous, but they are more than a cosmetic concern. They suggest that your venous circulation is under real strain.
This is often the point where people start to consider seeking medical advice. Perhaps the discomfort interferes with daily activities or exercise routines. Maybe you’ve tried compression stockings or elevating your legs at the end of the day, but you’re still experiencing aching and swelling. Even though the situation may not yet be severe, it’s an opportunity to talk with a healthcare professional who can help determine what’s going on and outline some options for halting or reversing the damage.
Intensifying Discomfort and Structural Changes
If varicose veins continue to progress without intervention, the condition can become more severe. By this stage, the veins are no longer just a cosmetic nuisance. They can cause persistent pain, more significant swelling, and a feeling of intense heaviness or fatigue in the legs. Tasks that used to be routine—like going for a walk, standing in line at the grocery store, or even sitting at a desk—might start to feel like a challenge. This is the point where people often realize that varicose veins are not just about looks. They can genuinely affect quality of life.
Chronic swelling may put pressure on the surrounding tissues. As a result, the discomfort tends to deepen, and people might notice that resting alone doesn’t solve the problem. In some cases, skin changes can begin here, too, signaling that the underlying venous insufficiency is starting to impact the body on a deeper level. The sooner you address these escalating symptoms, the better your chances of preventing lasting damage.
Skin Changes and Irritation
As varicose veins advance further, the skin around the affected areas may begin to show it. Discoloration—often a brownish or reddish tone—can appear as stagnant blood flow and increased pressure take their toll. You might also notice itching or irritation on the surface of the skin. These symptoms indicate that the problem isn’t just inside the vein anymore; it’s affecting the tissues around it. Chronic venous insufficiency can cause inflammation, dryness, and even a delicate thinning of the skin.
Though these changes can be uncomfortable and concerning, they also serve as an important signal. They’re urging you to seek treatment before the condition reaches a truly debilitating stage. With the right care and interventions at this point, it’s often possible to restore some balance to the veins and prevent the situation from escalating into more serious complications.
When Ulcers Enter the Picture
One of the most serious developments in advanced varicose veins stages is the appearance of venous ulcers. These often begin as small sores, usually around the ankles, that can be slow to heal. At first, they may be painful and unsightly but still treatable if addressed promptly. The problem is that these ulcers can easily become chronic wounds, healing partially only to return again later. Without timely intervention, they can grow larger, more painful, and prone to infection.
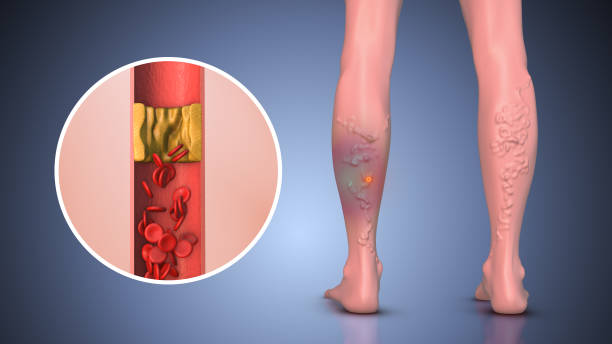
Open ulcers don’t heal properly because the circulation in the legs is so compromised that the body can’t deliver enough nutrients and oxygen to the skin. At this stage, medical attention is not just an option—it’s a necessity. Treating venous ulcers often requires a combination of therapies, from specialized wound care to procedures that improve blood flow. Ignoring these ulcers can lead to ongoing pain, infection risk, and reduced mobility.
Facing Advanced Stages and Non-Healing Ulcers
When venous ulcers fail to close and become persistent, the situation moves into a stage that poses substantial health risks. Infection becomes a constant threat, and day-to-day life can be overshadowed by pain, bandage changes, and doctor’s visits. This advanced venous insufficiency can severely limit mobility and independence. While it’s never too late to seek help, early intervention is always preferable. The right treatment at the right time can spare you from reaching this point.
Considering Treatment Options: When Surgery Makes Sense
Not everyone with varicose veins needs surgery. Many find relief through simple measures like wearing compression stockings, elevating their legs, exercising regularly, and maintaining a healthy weight. Medications can also help ease discomfort, while lifestyle changes may slow the progression of vein disease.
However, if these non-surgical methods aren’t providing enough relief or if you’re experiencing significant pain, swelling, or ulcers, it might be time to consider more advanced treatments. Minimally invasive procedures, such as keyhole surgery, address the root of the problem—truncal vein reflux. These surgeries involve small incisions and use techniques like radiofrequency or medical glue to seal off or remove affected veins. This redirects blood flow through healthier vessels, reducing pressure and alleviating symptoms.
Surgery may also be recommended if there’s a high risk of complications, such as bleeding or clot formation. Additionally, some people choose surgery for cosmetic reasons if varicose veins cause emotional distress. It’s important to balance these decisions with medical advice. Discussing your specific situation with a vascular specialist ensures you choose the most appropriate treatment based on your symptoms and overall health.
Struggling with Varicose Veins?
Explore safe and effective treatment options with Dr. Darryl Lim.

Moving Forward with Confidence
Nobody wants their varicose veins to escalate from a minor annoyance to constant discomfort. The good news is you have options. By understanding the stages of varicose veins—from mild varicosities to chronic ulceration—you can identify changes early and take action before things worsen.
Every person’s experience is unique, but proactive care is essential. Keep an eye on your legs, consult a healthcare professional when symptoms arise, and explore treatment options as needed. Whether it’s adjusting your daily habits, wearing compression stockings, or considering surgery, taking the right steps can lead to healthier, more comfortable legs.

















