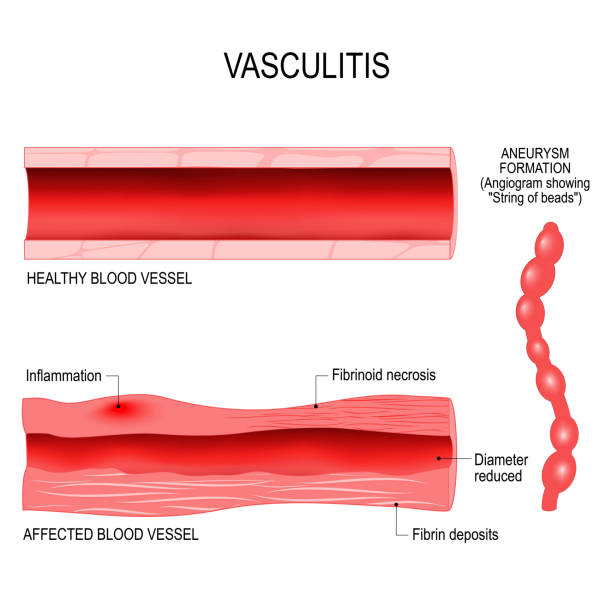
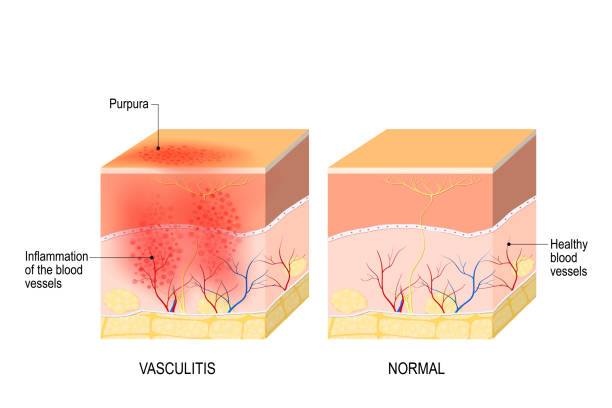
Hearing the word “vasculitis” for the first time can feel like stepping into unfamiliar territory. At its core, vasculitis means inflammation of the blood vessels, a condition that can affect people in many different ways. This inflammation may cause certain vessels to narrow, weaken, or become blocked, leading to symptoms that vary widely depending on which parts of the body are involved. Some individuals notice changes on their skin, such as unusual rashes or spots. Others may have joint pain, persistent headaches, fevers, or unexplained feelings of weakness that don’t seem to go away. There can also be numbness or tingling in the limbs, and in more severe situations, vital organs may suffer damage.
No two cases of vasculitis are exactly alike. In some people, it appears suddenly and improves with proper treatment. In others, it may be more stubborn, becoming a long-term issue that requires ongoing care. Understanding the nature of vasculitis can help lift some of the uncertainty, giving you a clearer sense of what you’re dealing with and what might come next.
Different Faces of the Same Condition
The word “vasculitis” does not refer to just one illness; rather, it’s a broad term that covers a range of conditions. Doctors usually classify them based on the size of the affected vessels and the underlying cause of the inflammation. Some are more common in older adults, while others may show up in children. Certain forms are associated with autoimmune disorders, where the body’s immune system mistakenly attacks healthy tissue. Others may arise after an infection, due to medication reactions, or in response to environmental exposures.
Large-vessel types, like giant cell arteritis and Takayasu’s arteritis, can involve some of the most important arteries in the body. Medium-vessel conditions, such as polyarteritis nodosa, often cause issues like skin lesions, muscle pain, and nerve involvement. Smaller-vessel problems, including granulomatosis with polyangiitis (formerly Wegener’s granulomatosis) and microscopic polyangiitis, may affect tiny vessels serving the lungs, kidneys, and other organs. There are also conditions seen in children—like Kawasaki disease—that primarily involve inflammation in medium-sized arteries and can lead to complications if not addressed promptly. Henoch-Schönlein purpura and eosinophilic granulomatosis with polyangiitis (formerly Churg-Strauss syndrome) are further examples, each with its own patterns of symptoms and progression.
The Importance of an Accurate Diagnosis
Because vasculitis takes so many forms, identifying which type you have can feel like solving a puzzle. Doctors often rely on a combination of diagnostic tools to get the full picture. Blood tests can reveal markers of inflammation or abnormal antibodies. Imaging studies, such as ultrasounds, CT scans, or MRIs, may show changes in blood vessels or organs. Sometimes, angiography—a specialized imaging technique that uses contrast dye—helps outline details that other scans might miss.
A biopsy remains a key step in many cases. This involves removing a small piece of tissue from the affected area and examining it under a microscope. By looking closely at the tissue, a pathologist can confirm if there’s inflammation, damage to the vessel walls, or other clues pointing to a particular type of vasculitis. While the idea of a biopsy might feel daunting, it can provide valuable answers that guide treatment decisions.
Treatment: Working Toward Relief and Control
Treating vasculitis isn’t always a matter of a quick fix, but it’s rarely a dead end either. The best approach depends on the underlying cause and how severely your vessels and organs are affected. When vasculitis stems from an infection, addressing that root problem often helps bring the inflammation under control. In cases where no single infection or trigger can be pinpointed, medications may be used to calm an overactive immune system.
Corticosteroids, for example, have long played a role in easing inflammation. Other immunosuppressive drugs may be added if necessary. While these medications can help prevent further damage, they come with their own risks and side effects. Your doctor will carefully weigh these considerations, possibly adjusting treatment as your condition changes. The goal is to reach a point where vasculitis becomes manageable, allowing you to maintain as normal a life as possible.
In some situations, vasculitis can lead to permanent damage, especially if organs were affected before treatment began. Even so, managing the disease can prevent new problems from emerging. With a thoughtful plan in place, many patients find ways to keep their condition in check and stop it from dominating their lives.
Finding the Right Specialist and Support
Vasculitis can be complicated, so working with a doctor familiar with your condition is important. The right specialist can explain test results, discuss treatment options, and monitor your progress. Asking questions and sharing concerns helps you stay involved in decisions about your care, making the process clearer and more reassuring.
Adjusting to Daily Life and Looking Ahead
Living with vasculitis often means adapting your routine. You may need to follow a set medication schedule, pay more attention to healthy habits, or watch for early signs that symptoms are returning. Over time, you’ll learn what works best for you. Connecting with others—friends, family, or support groups—can make you feel less alone and provide helpful coping strategies.
There may not be a perfect cure, but effective treatments and careful management can reduce the impact of vasculitis. By working closely with your healthcare team, you can find the right approach to keep symptoms in check and protect your long-term health. Over time, this condition can become more manageable, allowing you to move forward with your daily life.

















