Small aneurysms are usually watched with regular scans and risk control. Larger ones are repaired to prevent rupture. Two main options exist. EVAR places a stent graft inside the aorta through small groin cuts and usually means a shorter hospital stay and recovery. Open repair replaces the weak segment through an abdominal incision and has a longer recovery but excellent durability. Most centres use a treatment threshold around 5.5 cm for men and about 5.0 cm for women, or earlier if growth is fast or symptoms appear. If an aneurysm ruptures the outcome is often fatal, which is why timely repair matters.
Why treat an aneurysm at all
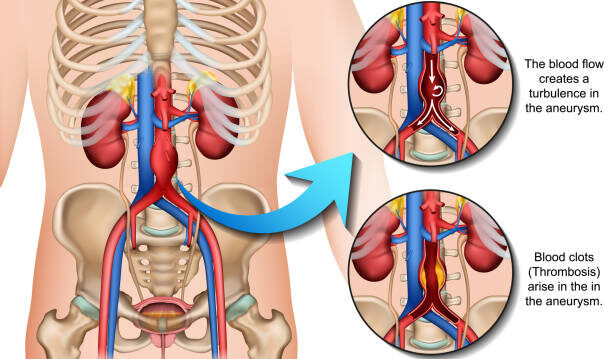
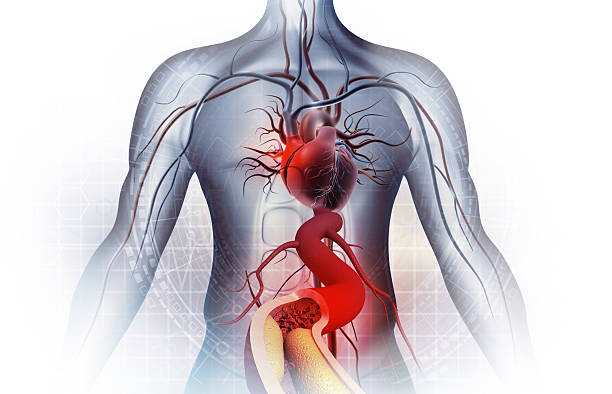
An aneurysm is a weak, stretched patch on the aorta. Left alone it keeps slowly enlarging. Think of blowing up a balloon. The larger it becomes, the thinner the wall gets and the more likely it is to pop. It is the same idea here. As the aneurysm grows, the chance of a tear or burst rises sharply. A rupture causes massive internal bleeding and is often fatal. Treating an aneurysm before it reaches that danger zone is how we prevent the emergency from ever happening.
When is repair recommended
No single number tells the whole story. Doctors look at four things together: size, how quickly it is growing, whether you have symptoms, and your overall health. The aim is to balance the risk of surgery against the risk of leaving the aneurysm alone for now.
Typical size and growth thresholds
For size, many centres offer repair once an abdominal aortic aneurysm measures about 5.5 cm in men and about 5.0 cm in women. Growth speed also matters: a jump of around 0.5 cm in six months or about 1.0 cm in a year will often bring treatment forward.
What counts as a symptomatic aneurysm
Symptoms can change the picture too. New or persistent deep abdominal pain, worsening lower back pain without another clear cause, a strong abnormal pulsation in the tummy, or tenderness over the aneurysm are all warning signs that the wall may be under stress. Occasionally, material inside the aneurysm (mural thrombus) can shed tiny clots downstream, causing a distal embolism. If a foot suddenly becomes painful, cold, bluish or purple at the toes, or if pulses in the foot feel weak or absent, urgent assessment is needed. Any sudden, severe abdominal or back pain with light-headedness or clamminess should be treated as an emergency.
Anatomy matters: fusiform versus saccular
Anatomy also counts- not all aneurysms have the same shape.
- Fusiform aneurysm: the aorta widens in a smooth, spindle-like way along a segment. Many AAAs are fusiform and are often suitable for standard surveillance (if size does not meet criteria) and, when needed, for EVAR or open repair.
- Saccular aneurysm: look more like a pouch on one side of the vessel. Because stress is concentrated, they can behave less predictably and may be repaired at smaller diameters, especially if symptoms are present or the wall looks irregular on CT.
Other anatomical details also guide timing and technique, for example how close the aneurysm sits to the kidney arteries, how long and straight the neck above the aneurysm is, the quality of the aortic wall, and the size and health of the iliac arteries in the pelvis.
How doctors weigh the decision
Finally, your overall health and goals are part of the decision. Heart, lung and kidney fitness, previous abdominal surgery, frailty, and how well you are likely to tolerate anaesthesia are weighed against the risk that the aneurysm will rupture in the coming years.
If the risk of rupture is higher than the risk of repair, treatment is usually recommended. If the aneurysm is small and slow-growing, and your health makes surgery particularly risky, careful surveillance with strong risk-factor control may be safer for now. Your surgeon will explain these trade-offs in plain terms and help you choose a plan that fits your health and priorities.
EVAR: Endovascular aneurysm repair
What it is. EVAR lines the inside of the aneurysm with a fabric-covered metal stent that is guided up from the groin arteries. The stent graft creates a new inner channel for blood, taking pressure off the bulging wall.
What to expect. In straightforward cases, EVAR is a shorter procedure with small cuts at the groin. People are usually sitting up the same day and walking with help the day after. Many go home within a couple of days and return to light daily activity within a week or two.
Strengths and considerations. EVAR typically means less pain and a faster recovery, which is helpful if you have heart or lung conditions. Not everyone’s anatomy is suitable, though.
The stent needs a good landing zone above and below the aneurysm to seal well. Lifelong imaging follow-up is important to check graft position and for any endoleak, which is when a little blood tracks around the graft. Many endoleaks are minor and simply monitored; a few need a touch-up procedure later.
Open surgical repair
What it is. Open repair replaces the diseased segment through an abdominal incision. The aorta is clamped above and below the aneurysm, the weak portion is removed, and a durable synthetic graft is sewn in. That graft becomes part of your aorta.
What to expect. Open repair is a longer operation and the hospital stay is typically a few days while pain settles and the bowels wake up. Recovery takes longer than with EVAR and builds steadily over several weeks.
Strengths and considerations. The long-term durability is excellent, with fewer reinterventions once you are healed. Open repair works well when anatomy is not suitable for EVAR. The trade-off is higher short-term surgical stress and a longer recovery window.
EVAR vs Open Repair: how your Vascular Surgeon decides
Choice of abdominal aortic aneurysm surgery is guided by three questions. Does your anatomy suit a stent graft with a reliable seal. What does your health suggest about the safety of each option. And what are your personal goals around recovery time and follow-up. Some people prefer the quickest recovery, others value the once-and-done stability of open repair.
There is no single “right” answer for everyone; the best approach is the one that matches your anatomy, your health and your priorities.
What if my aneurysm is small
Not all aneurysms need immediate repair, especially the smaller ones. Most are followed with scheduled ultrasound or CT scans while you work on risk control.
Stopping smoking, keeping blood pressure and cholesterol in range, staying active, and maintaining a healthy weight all help slow growth. Your team will shift from surveillance to repair if the aneurysm crosses the size threshold, grows quickly, becomes symptomatic, or develops features on imaging that raise concern.
What recovery looks like
After EVAR. Many people go home one to three days after surgery. Groin soreness settles over a few days, and light activity is usually possible within a week or two. You will have an imaging schedule to confirm the graft remains well-positioned and sealed.
After open repair. Discharge is commonly around five to seven days in uncomplicated cases. Tiredness and a healing incision are normal for a few weeks. Activity builds gradually with guidance from your team. Fewer long-term scans are needed than after EVAR because the graft is sewn in place.
Key facts worth remembering
- Repair is about preventing rupture, not treating symptoms alone
- Most centres use about 5.5 cm for men and 5.0 cm for women as a starting point for abdominal aneurysm repair decisions
- EVAR usually means a shorter hospital stay and quicker recovery
- Open repair has a longer recovery but excellent durability
- If rupture occurs, survival is poor, which is why timing matters
Conclusion
If your scan shows an aneurysm, ask your doctor about size, growth rate, and whether your anatomy suits EVAR. If you would like a guided discussion, you can book a consultation with Dr Darryl Lim, Vascular and Endovascular Surgeon. He will review your scans, explain your options in clear, simple language, and help you choose a plan that fits you best.