If your legs have been feeling heavier lately, or your varicose veins seem more obvious than they used to be, you’re probably not imagining it. A lot of people notice the connection between weight changes and leg symptoms long before they ever speak to a specialist.
So the question is a practical one- Can weight gain actually make varicose veins (or spider veins) worse?
Yes, often. But it’s not simply “more weight = more veins”. The real story is pressure, circulation mechanics, and how well your leg veins cope with day-to-day load.
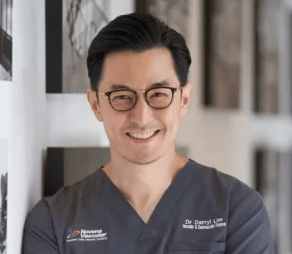
In this article, Dr Darryl Lim, a vascular and varicose vein specialist in Singapore, explains how weight gain affects vein function, what weight loss can and cannot fix, and the steps that genuinely reduce discomfort and protect long-term circulation.
Understanding Varicose Veins in Plain Terms
Varicose veins form when one-way valves inside the leg veins weaken. Normally, these valves help keep blood moving upward toward the heart. When valves fail, blood can fall backward (reflux), increasing pressure in the veins. Over time, veins stretch, enlarge, and become visible, often with symptoms such as
- Aching or throbbing legs
- Heaviness or fatigue that worsens through the day
- Swelling (especially around the ankles)
- Night cramps or restless legs
- Itching, burning, or skin irritation
- Skin discoloration near the ankles in more advanced disease
This sits under the umbrella of chronic venous insufficiency (CVI)– a progressive circulation issue that tends to worsen if reflux isn’t identified and addressed.
How Weight Gain Impacts Your Veins
Weight gain can worsen varicose vein symptoms through a few mechanisms. This can be explained as a “stacking effect”: more pressure, less efficient return, and less pumping action.
1) More pressure in the leg veins
Leg veins already work against gravity. Carrying extra weight increases pressure within the veins of the lower limbs. That matters because higher pressure can:
- Strain already-weak valves
- Push borderline veins into more obvious reflux
- Increase pooling and end-of-day swelling
- Make existing varicose veins look more prominent
In practical terms, people often describe symptoms that start earlier in the day after weight gain, and take longer to settle at night.
2) Higher abdominal/pelvic pressure and less efficient venous return
Excess abdominal and pelvic fat can increase pressure within the abdomen and pelvis. When that pressure is higher, blood return from the legs can be less efficient, and pooling becomes more likely.
This does not mean everyone who gains weight will develop varicose veins. But if you already have valve weakness or strong genetics, the added strain can shift symptoms from mild and occasional to disruptive.
3) Low-grade inflammation that makes symptoms feel worse
Weight gain (especially central weight gain) is associated with higher levels of chronic, low-grade inflammation. Inflammation doesn’t “create” varicose veins by itself, but it can worsen the environment in which vein disease progresses. Many patients describe more tenderness, heaviness, or swelling alongside weight changes.
4) Reduced mobility weakens the calf “pump”
Your calf muscles are not just for walking. They act like a powerful circulation pump. Every time you step, your calf squeezes the deep leg veins and pushes blood upwards.
When activity levels drop (which often happens with weight gain, knee/back pain, or just a busy routine), the calf pump becomes less effective, leading to:
- More pooling in the lower legs
- Increased ankle swelling
- Heaviness that builds through the day
- Varicose veins becoming more noticeable
This is one reason symptoms often improve on holidays (more walking) and worsen during sedentary weeks.
Why Your Varicose Veins Look Worse After Weight Gain
Some patients ask, “Are my veins actually getting worse—or do they just look worse? ”
Often, it’s both.
- Appearance effect: Weight gain can change how veins sit under the skin, making varicose veins look more prominent and spider veins easier to notice.
- Disease progression effect: Increased venous pressure can worsen reflux over time, leading to more symptoms and more visible vein changes.
- symptoms and more visible vein changes.
If you’re noticing more symptoms, not just a cosmetic change, that’s a stronger clue the underlying circulation problem may be progressing.
Can Weight Gain Cause Varicose Veins in the First Place?
Weight gain is usually not the sole cause. Varicose veins most commonly develop due to a combination of:
- Genetics (family history)
- Age-related valve weakening
- Hormonal factors (particularly in women)
- Pregnancy history
- Prolonged standing or sitting
- Prior clotting events or vein injury
- Excess body weight
In other words, weight gain is often a multiplier– it increases strain on a system that may already be predisposed to valve failure.

Will Losing Weight Make Varicose Veins Go Away?
This is where expectations need to be clear.
Weight loss can significantly improve symptoms.
Many patients notice meaningful improvement in:
- Swelling
- Heaviness
- Aching after long days
- Exercise tolerance
- Overall leg comfort
Reducing body weight can lower venous pressure and make daily movement easier- both of which help the venous system.
What weight loss usually cannot do
Weight loss does not “repair” damaged vein valves. If valves are already failing, weight loss alone usually cannot reverse that structural issue.
A simple analogy: it’s like a worn door hinge. Taking weight off the door helps, but the hinge may still not close properly.
That’s why some patients feel much better after weight loss but still have visible varicose veins (or recurring symptoms) because the reflux source is still there.
What most people don’t realise
Here is the part most people only learn after years of symptoms:
Varicose veins are not just surface veins. They are often a sign of a deeper valve problem that cannot be “out-dieted.” Healthy lifestyle changes are essential, but they are not a substitute for a proper vein evaluation when symptoms persist.
Practical Ways to Support Healthy Veins (Even Before Treatment)
If you are dealing with leg discomfort, visible varicose veins, or weight-related symptom flare-ups, these steps can help immediately.
Stay Active in Vein-Friendly Ways
Movement improves circulation and activates the calf pump. Helpful options include:
- Walking (most practical and effective)
- Cycling
- Swimming
- Elliptical training
- Yoga (especially calf/ankle mobility)
Consistency matters more than intensity.
Elevate Your Legs Daily
Elevate your legs above heart level for 15–30 minutes, especially after long periods of standing or sitting. This helps reduce pooling and swelling.
Use Compression Stockings When Appropriate
Compression stockings can reduce swelling and heaviness by supporting upward blood flow. They do not fix valve failure, but they can improve daily comfort and support outcomes after treatment.
Build a Vein-Supportive Eating Pattern
No “magic food” cures varicose veins, but nutrition can reduce pressure and swelling by supporting weight control and circulation:
- Increase fiber (helps reduce straining and pressure)
- Stay well-hydrated.
- Moderate salt intake (can reduce swelling)
- Emphasize fruits/vegetables (flavonoid-rich choices are often recommended for vascular support).
- Prioritize protein for healthy activity and weight management
Break Up Long-Standing or Sitting
If your work demands standing or desk time, aim for short “circulation breaks”:
- Calf raises (10–20 reps)
- Ankle pumps
- Short walks every 30–60 minutes
Need an expert vascular opinion for your Varicose Veins?
Book an appointment with Dr. Darryl Lim today and get a personalized treatment plan.

When to See Dr. Darryl Lim for a Vein Evaluation
It is time to consider a professional assessment if you experience any of the following:
- Daily leg heaviness or aching that worsens later in the day
- Persistent ankle swelling
- Night cramps or restless legs
- Itching, burning, or tenderness along visible veins
- Skin darkening or thickening near the ankles
- Visible varicose veins with discomfort
- Symptoms that worsen after weight gain (even modest gain)
A key advantage of early evaluation is clarity: you learn whether your symptoms are primarily vein-related and what level of treatment (if any) is appropriate.
A quick safety note
If you ever develop sudden one-sided leg swelling, redness/warmth, severe calf pain, or new shortness of breath/chest discomfort, seek urgent medical assessment. Those symptoms are uncommon, but they should not be ignored.
What a Proper Vein Assessment Should Include
A proper evaluation involves more than a visual inspection. The gold standard assessment utilizes a duplex ultrasound to determine:
- Vein valve function
- Reflux (backward flow)
- Which veins are diseased vs healthy
- The true source of symptoms
This matters because treating only what you can see may not address the underlying reflux source. Treating the cause is what leads to more durable relief.
If Lifestyle Changes Aren’t Enough: Modern Treatment Options
When varicose veins are driven by reflux, modern treatments are designed to close off or eliminate diseased veins so blood reroutes through healthier pathways. These are typically minimally invasive outpatient procedures and may include:
- Endovenous thermal ablation (Radiofrequency Ablation)
- Medical adhesive closure (VenaSeal)
- Ultrasound-guided Sclerotherapy
- Microphlebectomy for bulgy varicose veins
The right option depends on ultrasound findings, symptoms, and your anatomy.
Takeaway: Weight matters, but it’s not the whole story
Weight gain can make varicose veins worse. It can increase pressure in the legs, reduce efficient blood return, and worsen symptoms like swelling and heaviness.
But weight isn’t a moral judgment or a single cause. Varicose veins are usually the result of valve dysfunction, genetics, and time- made more symptomatic by increased pressure. Weight loss can meaningfully improve comfort and reduce progression risk, but damaged valves may still require medical treatment for lasting relief.
If your symptoms are increasing, the most useful next step isn’t guessing. It’s getting a clear diagnosis and a plan built around your circulation.
Frequently Asked Questions
1) Can weight gain really make my varicose veins worse?
Yes. Extra weight increases pressure in the leg veins, making it harder for valves to function properly and often worsening venous insufficiency symptoms such as swelling, heaviness, and pain.
2) Will losing weight make my varicose veins disappear?
Weight loss can reduce swelling and heaviness and may make veins less prominent. However, it typically cannot repair damaged vein valves. If reflux is present, symptoms may persist until the underlying issue is treated.
3) How much weight loss makes a difference?
Even modest, sustainable weight loss can reduce venous pressure and improve symptoms. The biggest benefit usually comes from combining weight improvement with consistent movement to strengthen the calf pump.
4) When should I see a specialist?
If you have persistent leg pain, swelling, heaviness, skin changes near the ankles, or visible varicose veins with symptoms (especially if symptoms are worsening), an ultrasound-based evaluation is recommended.