What is Peripheral Vascular Disease?
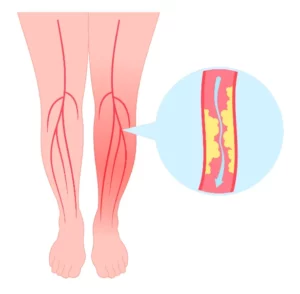 Peripheral Vascular Disease (PVD), sometimes also referred to as peripheral artery disease (PAD), is a relatively common but potentially serious condition that affects blood vessels located outside the heart and brain. These peripheral arteries and veins are responsible for transporting blood throughout the body—particularly to the limbs. When they become narrowed or blocked, blood flow to certain areas can be substantially reduced. In many cases, the problem lies in the arteries of the legs and feet, where a buildup of fatty deposits (known as atherosclerosis) can impede circulation.
Peripheral Vascular Disease (PVD), sometimes also referred to as peripheral artery disease (PAD), is a relatively common but potentially serious condition that affects blood vessels located outside the heart and brain. These peripheral arteries and veins are responsible for transporting blood throughout the body—particularly to the limbs. When they become narrowed or blocked, blood flow to certain areas can be substantially reduced. In many cases, the problem lies in the arteries of the legs and feet, where a buildup of fatty deposits (known as atherosclerosis) can impede circulation.
Recognizing Possible Symptoms
Many people first notice PVD when they experience leg discomfort during physical activities such as walking or climbing stairs. This symptom, often called claudication, may manifest as cramping or a heavy, tired feeling in the legs that eases with rest. Some individuals also find that one foot or leg feels colder than the other, or that skin color changes—like paleness or a bluish tinge—become more obvious.
Persistent numbness or weakness, as well as slow-healing sores on the feet or legs, can also signal circulation problems. You might observe that hair growth on the affected limb diminishes, and toenails appear to grow more slowly. If any of these signs or symptoms occur and don’t improve, it’s generally wise to see if PVD could be the underlying cause.
What Causes PVD?
Atherosclerosis is the most common culprit in Peripheral Vascular Disease, wherein fatty plaques accumulate along artery walls, causing them to narrow and stiffen. Several other factors can raise the risk of developing PVD, including diabetes (which can damage blood vessels), high blood pressure (which weakens artery walls), and smoking (which accelerates atherosclerosis).
Elevated cholesterol levels contribute to plaque formation, while being overweight or sedentary puts extra pressure on the cardiovascular system. Increasing age—particularly after 50—also plays a role, as does having a family history of circulatory problems. Certain conditions, like kidney disease or inflammation of the blood vessels (vasculitis), may also be involved.
Complications of Peripheral Vascular Disease
Reduced blood flow to the limbs can lead to a variety of challenges:
- Claudication: Pain or cramping in the calves, thighs, or buttocks during exercise.
- Non-Healing Wounds: Minor cuts or sores may heal slowly or become infected due to poor circulation.
- Critical Limb Ischemia: Extremely reduced blood flow can result in tissue damage, and potentially gangrene, if left untreated.
- Cardiovascular Risks: PVD often indicates a more generalized circulatory problem and can increase the likelihood of heart attack or stroke.
- Quality of Life Concerns: Fear of triggering pain can reduce mobility, and the chronic stress of dealing with persistent leg discomfort may affect emotional well-being.
How is PVD Diagnosed
Evaluating suspected PVD often begins with a physical exam. A healthcare provider checks for diminished pulses in your legs or feet and looks for other signs, such as skin changes. The Ankle-Brachial Index (ABI) is a common initial test, comparing blood pressure in your ankle to that in your arm to detect reductions in leg circulation.
Two additional imaging methods frequently come into play for a closer look:
- Doppler Ultrasound is a non-invasive procedure that uses sound waves to map blood flow in your arteries, helping pinpoint narrowing or blockages and gauge the severity of any vascular disease.
- CT Angiography (CTA) involves using contrast dye and specialized X-ray technology to create detailed cross-sectional images of the blood vessels. This modality can be particularly helpful for identifying and locating more complex or extensive blockages, especially in deeper lying arteries (for example the arteries in the abdomen).
By combining these assessments, healthcare providers can build a comprehensive understanding of your vascular health and plan an appropriate course of action.
Approaches to Treatment
If you’re diagnosed with PVD, the ideal treatment depends on both the extent of the disease and any underlying conditions. Sometimes lifestyle adjustments—like quitting smoking, adopting a healthier diet, and increasing low-impact exercise—provide noticeable improvement. Medications may also be prescribed to manage blood pressure, lower cholesterol, or reduce blood clot formation.
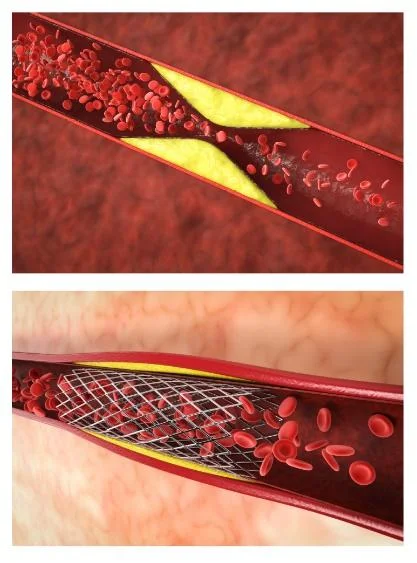
For more significant blockages, minimally invasive interventions such as angioplasty or stenting can reopen narrowed arteries and restore blood flow. In advanced or complex cases, bypass surgery may be recommended, creating a new route around a blocked artery. Treatment plans vary from patient to patient, aiming to address both symptom relief and long-term vascular health.
Staying Ahead of PVD
Early identification and thorough management can profoundly benefit individuals with Peripheral Vascular Disease. Although PVD can be serious, many people continue to lead active, fulfilling lives by staying engaged with their treatment plans, making key lifestyle changes, and adhering to any prescribed medications. Regular follow-up appointments offer a chance to monitor progress, catch potential complications before they become severe, and adjust treatments if necessary.
If you have concerns about PVD or would like tailored guidance for your vascular health, Dr. Darryl Lim provides a compassionate and personalized approach to care. His extensive expertise in minimally invasive interventions can help you find the most effective solutions for your situation.
Disclaimer: The information above is intended for general reference and should not replace individualized medical advice. Always consult a qualified healthcare professional for recommendations suited to your specific needs.
FAQ about Peripheral Vascular Disease
Peripheral Vascular Disease (PVD) is a blood circulation disorder, where blood vessels outside the heart—usually the arteries—experience narrowing or blockage, often affecting the legs and feet. This typically occurs due to atherosclerosis, a build-up of fatty deposits (plaque) on the vessel walls, leading to reduced or obstructed blood flow.
Anyone can develop PVD, but it’s more common in people over 50, smokers, diabetics, and those with high blood pressure or high cholesterol. Early detection and treatment is the best way to slow down progression of the disease and reduce your chances of irreversible tissue loss.
If you’re experiencing leg pain while walking, numbness, or sores that aren’t healing, you might have PVD. But don’t worry – Dr. Lim is here to help diagnose and treat your condition, getting you back on your feet in no time!
To diagnose PVD, Dr. Lim might recommend a range of tests like an ultrasound, blood tests, or an angiogram. These are pretty straightforward and will help in crafting your treatment plan by identifying which blood vessels are blocked and how severe the blockage is.
Poorly healing wounds can be a sign of reduced blood flow due to PVD, especially in patients suffering from diabetes. Patients with diabetes also often have diminished sensation in their feet due to nerve damage (neuropathy), making them more likely to injure themselves. It’s crucial to get these issues checked by a professional as early as possible to reduce your chances of further issues like infection, gangrene and irreversible tissue loss.
While there’s no magic bullet to ‘cure’ PVD, it can be very manageable. Lifestyle changes, medication, or sometimes surgery can help control the symptoms and improve your quality of life.
If you have been recently diagnosed with PVD, do not be afraid. Dr. Lim will guide you through the best treatment options for your situation and help you gain control over your health and body.
Treatment plans depend on the severity of your symptoms, amount of tissue damage and the extent of infection (if any).
General treatment plans typical include lifestyle changes, medications to optimize the treatment underlying conditions, medications to improve blood flow, and sometimes procedures to open blocked vessels. Dr. Lim has a wealth of knowledge and experience with complex angioplasties to help you and your loved ones obtain the best possible outcomes.
Dr Lim works closely with other doctors and allied health professionals, like endocrinologists, renal physicians, podiatrists and physiotherapists, to help his patients get back on their feet as soon as possible. Sometimes it may also be necessary for patients to speak to a dietician or nutritionist to help design a sustainable meal plan.
It can be frightening to hear the word “amputation,” but there may be options like revascularization procedures to improve blood flow and promote healing. Dr. Lim specializes in these life- and limb-saving techniques and will explore every possibility to help you. Remember that early treatment for infections or tissue damage is usually your best chance of avoiding irreversible tissue loss and seek medical advice as soon as possible.
It’s tough when loved ones avoid medical advice. In our experience, one of the best ways to help a loved one who refuses to seek medical treatment is to understand their personal barriers to seeking care. This conversation may be difficult to initiate as your loved one may be worried about having their views ridiculed or dismissed. Take their concerns seriously and show them that you understand and are hearing them. You can also take some time to understand their diagnosis to the best of your ability, in case they do not understand it and need it to be explained to them again.
Some reasons patients may avoid medical advice or treatment are 1) Fear of bad news, 2) Poor understanding of the disease or diagnosis, and, 3) Worries about being a ‘burden’ to their family (financially, physically etc.).
A lower limb angioplasty is a procedure to open up narrowed or blocked blood vessels in your legs, improving blood flow. It can relieve pain and help heal wounds. This is a minimally invasive procedure that requires a ‘puncture’ (injection) in your groin. Dr. Lim has successfully performed many of these procedures, helping patients regain their mobility and quality of life.
Angioplasty is a common treatment where a small balloon is inserted into a narrowed artery and inflated to improve blood flow. A stent may also be placed to keep the artery open. This helps relieve leg pain and other symptoms caused by poor circulation.
The main cause of peripheral vascular disease (PVD) is atherosclerosis- when fatty deposits build up in the arteries, narrowing them and reducing blood flow. Smoking, diabetes, high blood pressure, and high cholesterol all increase the risk.
Leg pain when walking, numbness, cold feet, slow-healing wounds, or skin discolouration may be early signs of peripheral vascular disease. These symptoms suggest poor circulation and should be evaluated by a vascular surgeon to prevent serious complications.
Peripheral vascular disease isn’t completely curable, but it can be managed effectively. Lifestyle changes, medication, and procedures like angioplasty can improve symptoms and reduce risks. Early diagnosis and treatment by a vascular surgeon are important for long-term care.
Vascular leg pain isn’t completely curable, but it can be well managed. Lifestyle changes, medication, and procedures like angioplasty can improve circulation and ease symptoms. Early evaluation by a vascular surgeon helps prevent complications.
Vascular pain often worsens with walking and improves with rest (claudication), while muscular pain may occur with movement or after exercise and improves with stretching or rest. If the pain is persistent or limits walking, it’s best to see a vascular surgeon for a proper assessment.
Yes, walking is highly beneficial for vascular disease. It improves circulation, strengthens leg muscles, and eases symptoms like claudication. Regular walking encourages better blood flow and may slow disease progression. Check with your doctor before starting an exercise routine.










