
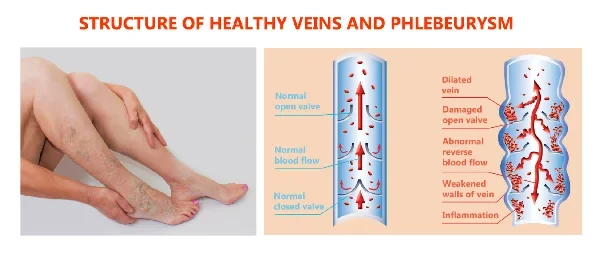
What is Venous Reflux?
Venous reflux, sometimes referred to as chronic venous insufficiency (CVI), is a condition in which the valves in the leg veins fail to function properly. In a normal circulatory system, these valves open to allow blood to flow upward toward the heart and then close to prevent it from flowing backward. When these valves weaken or become damaged, blood can reverse direction (reflux) and pool in the leg veins. This excessive pooling of blood increases venous pressure, leading to a variety of symptoms, from mild leg discomfort to more severe complications such as venous ulcers.
Why Venous Reflux Matters
When venous valves cannot adequately move blood back to the heart, the body must work harder to maintain healthy circulation. Over time, chronic back flow may cause persistent swelling, pain, and changes in skin pigmentation. These effects can significantly impact your day-to-day activities and quality of life, limiting mobility and potentially leading to more complex medical issues. Recognizing early warning signs and seeking prompt treatment can help prevent the condition from progressing to advanced stages.
Common Signs and Symptoms
Venous reflux manifests differently in different individuals, but some of the most frequently observed signs and symptoms include:
- Swelling in the legs or ankles
- Spider and reticular veins, which are smaller visible veins near the skin’s surface
- Varicose veins, often appearing as bulging or rope-like veins
- Heavy, restless legs, especially after prolonged standing or sitting
- Aching, throbbing, or cramping leg pain that may worsen later in the day
- Itchy or irritated skin, particularly near prominent veins
- Brownish skin discoloration, commonly around the ankles
- Ulcers or open sores, typically forming in the lower leg or ankle region
Not all individuals will experience every symptom, but any persistent leg discomfort or noticeable change in skin appearance warrants a professional assessment to rule out or confirm venous reflux.
Underlying Causes and Risk Factors
Venous reflux can affect both men and women, although it is often more prevalent among women due to hormonal influences and pregnancy-related vascular changes. One of the most common causes is age-related degeneration of the vein walls and valves. Over time, these structures naturally weaken, making it easier for blood to flow backward. Other risk factors include:
- Family History: A genetic predisposition to varicose veins or other venous conditions can increase your likelihood of developing venous reflux.
- Pregnancy: Hormonal changes and an enlarged uterus can elevate venous pressure in the legs, leading to or exacerbating reflux.
- Obesity: Excess weight applies added strain on the leg veins, making it harder for blood to travel upward.
- Physical Inactivity: Lack of regular exercise can reduce muscle contractions in the calves that help pump blood back to the heart.
- Prolonged Standing or Sitting: Occupations that require one to stand or sit for long hours can contribute to venous stasis, in which blood pools in the legs instead of circulating efficiently.
Potential Complications if Left Untreated
Without timely intervention, venous reflux may progress to more serious complications that affect both the appearance and health of your legs. Chronic back flow of blood can lead to:
- Progressive Skin Changes: Persistent venous congestion often causes discoloration or thickening of the skin.
- Stasis Dermatitis: Inflammation or eczema-like changes in the skin around the ankles and lower legs.
- Lipodermatosclerosis: Hardening or tightening of the skin and subcutaneous tissues.
- Venous Ulcers: Open wounds around the ankles that can be painful and slow to heal.
These issues can dramatically reduce quality of life and require more intensive treatment once they have developed, which is why early diagnosis is so crucial.
Diagnosis and Assessment
To confirm a diagnosis of venous reflux, your vascular surgeon will usually begin with a thorough physical examination of your legs, looking for visible signs such as swelling, varicose veins, or skin changes. An duplex ultrasound is commonly the next step. This painless, non-invasive test uses sound waves to visualize the flow of blood within the veins, pinpointing areas where reflux occurs and determining the degree of valve dysfunction.

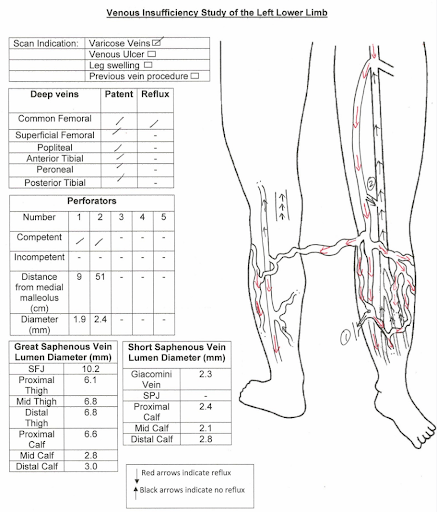
Duplex Ultrasound Scan to evaluate for
- Presence of venous reflux
- Locations of reflux (superficial, deep, perforating veins)
- Size (diameter) of veins
- Presence of DVT
In certain situations, a CT (Computed Tomography) scan of the abdomen or pelvis may also be recommended to rule out compression or blockage of the pelvic veins, which can worsen symptoms in the lower extremities. By combining clinical evaluation with imaging studies, vascular specialists can create a customized treatment plan tailored to your specific needs.
Treatment Options
The primary objective of any venous reflux treatment is to minimize the backward flow of blood and improve overall circulation. Depending on the severity of your symptoms and any underlying causes, your surgeon may recommend one or more of the following approaches:
- Compression Therapy
Prescription-grade compression stockings apply controlled pressure on the legs, encouraging venous blood to flow upward. The stockings come in various pressure levels, and higher grades typically require a proper medical fitting to ensure patient safety and comfort. However, in humid climates like Singapore, compliance with this therapy may be low. - Lifestyle and Activity Modifications
Incorporating regular exercise—such as walking, cycling, or swimming—can significantly aid calf muscle function, promoting blood flow. Maintaining a healthy weight and avoiding prolonged immobility also help reduce venous pressure. - Medications
While some medications may alleviate swelling or discomfort, venous reflux is primarily structural in nature. Therefore, medication alone often provides only partial relief. However, it can be useful as an adjunct therapy in managing mild symptoms or inflammation. - Minimally Invasive Procedures
Minimally invasive treatments have become the cornerstone of modern venous care. Approaches like Sclerotherapy, Radiofrequency Ablation (ClosureFast™), VenaSeal (medical glue), Endovenous Laser Ablation, and Clarivein (pharmacomechanical ablation) help seal or remove affected veins with minimal downtime. These procedures are typically performed under local anesthesia, offering patients faster recovery and excellent success rates. - Surgical Intervention
In advanced cases, or when minimally invasive options are less suitable, traditional surgery may be needed. Vein stripping, through a small incision near the groin, removes large segments of diseased veins. While surgery is more invasive than other treatments, it can be highly effective for patients with extensive varicose veins.
Prevention and Management
Managing venous reflux over the long term involves a combination of timely treatment, proactive lifestyle measures, and routine check-ups. Patients can significantly slow or even halt disease progression by:
- Staying physically active and performing exercises that engage the calf muscles
- Maintaining a healthy body weight
- Wearing compression stockings as prescribed
- Elevating the legs when resting to reduce swelling
- Attending regular follow-up appointments with a vascular specialist
If you notice any new or worsening symptoms—such as persistent pain, changes in skin color, or the development of sores around your ankles—contact your healthcare provider right away. Early detection and prompt intervention remain key to preventing minor issues from escalating into serious complications.
Conclusion
Venous reflux is a common yet manageable condition, provided that it is recognized and treated appropriately. Whether you’re dealing with superficial venous reflux, deep venous reflux, or both, a combination of conservative measures, minimally invasive procedures, and—in certain cases—surgical intervention can greatly improve symptoms and quality of life. If you suspect you may have venous reflux or have been experiencing persistent leg swelling, pain, or skin changes, do not hesitate to seek professional guidance. Early intervention is essential for maintaining healthier veins and preventing more serious complications over time.
Disclaimer: This information is provided for educational purposes only and should not replace professional medical advice. Always consult a qualified healthcare provider for personalized assessment, diagnosis, and treatment recommendations.
FAQ about Venous Reflux
Our veins have small, one-way valves that keep blood flowing towards our heart. Sometimes, these valves can become weakened or damaged, and they don’t close properly. When this happens, blood can flow backward and pool in the veins, and this condition is what we call venous reflux.
It often occurs in the legs and can lead to symptoms like pain, swelling, and varicose veins. Dr. Lim has extensive experience in managing this condition and will work with you to find the most effective treatment options to manage any discomfort or complications.
Varicose veins and venous reflux are related, but they aren’t quite the same thing. Venous reflux is the underlying condition where, as we mentioned, the blood flows backward due to faulty valves and pools in the veins. When this happens, it can cause the veins near the surface of the skin to become swollen, twisted, and visible, and these are what we call varicose veins. So, you can think of varicose veins as a possible symptom or result of venous reflux.
Dr. Lim can help clarify any concerns or queries you have about these conditions and discuss potential treatments if you’re experiencing discomfort or other issues.
Varicose veins are enlarged, twisted veins that are visible under the surface of the skin. They often appear in the legs and can cause discomfort, pain, or swelling.
Spider veins are smaller, more superficial veins that often appear as blue, purple, or red lines on the skin surface. They are typically not painful but can be cosmetically bothersome to some individuals.
Several factors contribute to the development of varicose and spider veins, including age, genetics, hormonal changes, pregnancy, obesity, and prolonged periods of standing or sitting.
While spider veins are generally harmless, varicose veins can sometimes lead to complications such as bleeding, blood clots, and ulcers. It is advisable to consult with a healthcare provider for diagnosis and treatment options.
Approximately half of the population has some form of venous disease while varicose veins affect one out of two people age 50 and older, and 15-25% of all adults. On average 18% of men and 25% of women develop varicose veins. Varicose veins are one of the most common venous issues affecting the world today.
Anyone can develop spider or varicose veins, but they are more common in those above 50 years old, females, individuals with a family history, and those with certain lifestyle factors like a high BMI, desk-bound work environments, or in occupations which require you to stand for long periods of time.
Here are some physical symptoms of varicose veins that make them easier to diagnose:
- Itchy or flaky skin around the affected vein, sometimes accompanied by a burning sensation,
- Feeling of heaviness or ache in the lower legs after standing or sitting for long periods of time (usually worse at end of day, with comparative relief in the morning),
- Muscle cramps or pain in the lower legs, and,
- Swelling around the ankles – the ankle area appears puffy and swollen, and the ankle bone may not be visible
Not all of these symptoms are present in the same person. However, if you fit the above description, or if you have one or more of these symptoms, it is likely you have varicose veins. These symptoms can take a toll on your quality of life, making it hard to do things like walking or even standing for long periods.
Fortunately, modern minimally-invasive surgical methods have made the treatment of varicose veins quick and easy. Feel free to reach out for a personalised assessment and consultation should you have any of the above concerns.
While not all people present with severe symptoms, varicose veins generally worsen over time. Initially, slight heaviness and discomfort in the affected leg will be felt. If untreated, this pain may increase and result in limitations in walking and cramping during the night. Eventually, varicose veins can lead to skin discolouration or open wounds (ulcers) around the ankles.
Your healthcare provider will usually diagnose these conditions based on a physical examination. Additional tests like ultrasound may be recommended to assess the presence of venous incompetency (reflux), and rule out other issues.
An ultrasound is the most common diagnostic test for varicose veins. Some patients may require a CT (Computed Tomography) scan of your abdomen may be indicated to evaluate for compression of your pelvic veins.
Treatment options may include lifestyle changes, compression stockings, minimally invasive procedures like sclerotherapy, radiofrequency ablation therapy, and surgical interventions like vein stripping.
Generally, spider veins are treated with less invasive methods like injection sclerotherapy or radiofrequency treatment. Spider veins usually require a few sessions of sclerotherapy to resolve.
Varicose veins may additionally require more extensive treatment like mini-stab avulsions (for removal) depending on their extent and severity.
Coverage varies by insurance provider and plan. It is essential to consult your insurance to determine what treatments are covered, especially since some treatments may be considered cosmetic.
Clinical results have been published documenting the success of Endovenous Radiofrequency Ablation, ClariVein and VenaSeal at above 90% and Sclerotherapy between 60-80%.
As with any medical treatment, each method has its own risks and benefits. Your surgeon will explore the most suitable treatment option, after a thorough assessment of your condition.
Sclerotherapy is commonly used to treat spider veins (small superficial veins) and has been used with safety and success since the 1930’s. This treatment is a non-surgical procedure, and can be performed in the outpatient clinic.
Using a very fine needle, a solution is injected into the vein. This solution causes the vein walls to stick together and eventually close. The obliterated vein is absorbed by the body over time.
Following sclerotherapy, there is very little to no downtime. Patients will be required to wear a compression stocking for the next week. They can return to work or carry on with normal activities straight away. Some patients may experience gentle bruising at the treated area, especially those with thin and lighter skin.
Patients should wait at least three months after pregnancy before being treated for venous insufficiency. Patients who have suppressed immune systems, deep vein thrombosis, and patients who are immobile (ie cannot walk or move around), are generally not good candidates for treatment and will require further evaluation to assess their suitability.
Recovery depends on the treatment method used. Minimally invasive treatments usually have shorter recovery times. Most patients will be able to walk on the same day after their surgery. Traditional open surgical treatments (eg open stripping of vein) may require a longer period for full recovery.
Yes. There is a possibility that new varicose or spider veins may develop over time even after successful treatment, particularly if underlying risk factors are not addressed. Risk of recurrence is usually around 5-10%.
This depends on the type of treatment you undergo. For minimally invasive treatments, most people can return to normal activities relatively quickly in a day or two. Vigorous exercise is usually not recommended till 2 weeks post-surgery. Traditional open surgical treatments may require a longer period for full recovery.
Most treatments aim to reduce the appearance and symptoms of varicose and spider veins significantly, but results can vary from person to person.
While many people seek treatment for cosmetic reasons, treatment can also alleviate symptoms like pain, swelling, and itching associated with varicose veins.
You can schedule a consultation by:
- Calling our clinic at +(65) 6694-2282,
- Leaving us a Whatsapp message +(65) 9727-0788,
- Emailing contact@drdarryllim.com, or
- Using our contact form [go to contact page]
During your first consultation, your vascular surgeon will examine your veins, discuss your symptoms, go over your medical history, and possibly recommend additional tests. A personalized treatment plan will then be discussed.
Venous reflux is often treated with vein ablation- a minimally invasive procedure that seals off faulty veins and redirects blood to healthier ones. This improves circulation and helps relieve symptoms like leg pain, swelling, and varicose veins.
Yes, venous reflux can cause leg pain. Faulty vein valves lead to poor circulation, resulting in aching, cramping, swelling, heaviness, or visible veins like varicose and spider veins. If untreated, symptoms may worsen over time and affect daily comfort and mobility.
Venous reflux doesn’t go away on its own and may worsen over time. However, it can be managed with early treatment, including lifestyle changes, compression stockings, and minimally invasive procedures to address the underlying vein issues and improve symptoms.
Venous reflux isn’t reversible, as damaged valves can’t be repaired. However, it’s highly treatable. Procedures like vein ablation can close off faulty veins, improve blood flow, and relieve symptoms. Early treatment helps prevent complications like leg ulcers or blood clots.
Massage may help relieve leg swelling or discomfort from venous reflux by improving fluid movement. However, it doesn’t fix the faulty valves causing the issue. It’s best used as a supportive therapy alongside proper medical treatment for lasting results.
Vein reflux is diagnosed with a duplex ultrasound, which checks for backward blood flow in your leg veins. If this reflux lasts longer than 0.5 seconds, it may indicate venous insufficiency. The scan helps assess severity and guide treatment options.
Yes, walking helps improve circulation and strengthens calf muscles, which assist in pumping blood back to the heart. Regular movement can ease symptoms like leg heaviness and swelling, making it a simple but effective way to support vein health.
Niacin (vitamin B3) supports vein health by improving blood flow, reducing inflammation, and lowering cholesterol. It’s found in foods like chicken, tuna, and peanuts. While helpful, always check with your doctor before starting any new supplements.
Yes, drinking water supports healthy circulation by helping your blood flow more easily. While over hydration may cause swelling in some cases, staying well-hydrated generally helps reduce blood pooling in the legs and supports overall vein health.










