Spider Veins: Symptoms, Treatments & Surgery
Spider veins are fine red or blue veins on the legs or other parts of the body. They typically fan out across the skin like small webs, and are also known as telangiectasias.
The answer to how to cure spider veins depends on their cause. Some cases are largely cosmetic, whereas others may be linked to issues like venous reflux. In general, spider vein treatment or management is best when performed early to prevent the condition from worsening.
What Are Spider Veins?
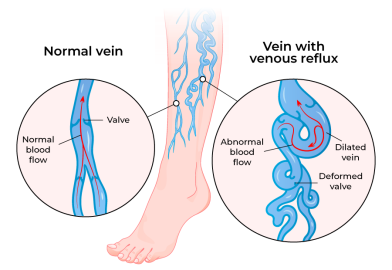
Spider veins usually appear as small, superficial veins. Compared to varicose veins, they don’t bulge outwards. However, they can still be signs of problems like venous reflux, which occurs when deeper veins allow blood to flow backwards.
Spider Vein Symptoms

While this condition is often more of a cosmetic issue, some symptoms suggest another condition may be involved:
- Subtle sting or itch after long hours on your feet
- Evening ankle puffiness that settles overnight
- Patches that darken or creep outward over a few months
- Night-time calf cramps, especially if varicose veins are also present
Diagnosing the Root Causes
Spider veins can often be identified through a simple visual examination, but in some cases, they may be linked to venous reflux (leaky valves in the veins). To check for this, a venous duplex ultrasound scan is usually performed. This is a painless and non-invasive test that can show:
- Whether venous reflux is present
- The locations of reflux (superficial, deep, or perforating veins)
- The size (diameter) of affected veins
- The presence of any deep vein thrombosis (DVT)
By identifying the underlying causes, we can recommend the most appropriate and effective treatment approach for you.
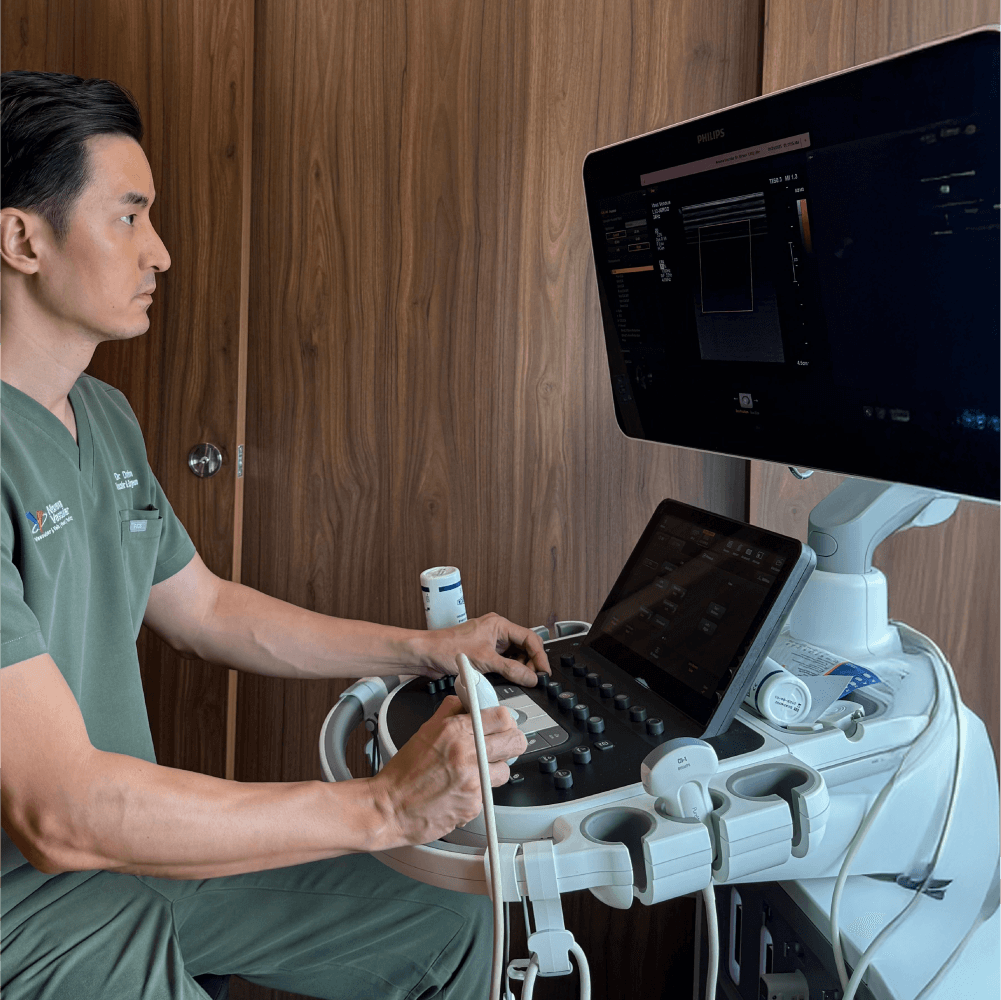
Get a Clear Diagnosis from a Specialist
Our doctor can help assess your condition with a quick and painless vein scan and guide you through your treatment options from there.
Spider Vein Treatments
Spider vein treatment depends on how extensive and large the veins are.
If a venous duplex ultrasound scan shows underlying truncal vein reflux (a deeper vein issue), treatment of the refluxing vein may be advised in addition to spider vein treatment. This combined approach often provides more effective and longer-lasting results.
For spider vein treatment on its own, most people usually need 1-3 sessions, spaced about 8-12 weeks apart, to allow proper healing and achieve the best cosmetic outcome.
If your ultrasound reveals underlying venous reflux, we can often seal the leaky vein and treat the surface spider veins in the same session. Minimally invasive techniques are available for this, such as Radiofrequency Ablation (RFA) or ClariVein®.
All treatments are performed or recommended by Dr Darryl Lim, who is experienced in minimally invasive interventions. Below are some of the common treatment options for spider veins:
Ideal for: Most leg spider veins
How it works: A fine needle is used to inject a small dose of sclerosant into the vein, which causes it to collapse. Over time, the vein is reabsorbed and gradually fades.
The session will take around 30-45 minutes, with most patients describing the sensation as a mild pin prick or slight burning that quickly subsides. Bruising or mild redness may occur, usually clearing in a week or two.
Ideal for: Very fine thread-veins or telangiectasia that are too small for injection
How it works: A hair-thin probe releases a split-second burst of radiofrequency energy to the vein, instantly closing it. The treated vein fades almost immediately.
The procedure takes 15-30 minutes, depending on the number of vessels. Most patients describe the sensation as a quick zap or pin prick. There is typically no downtime, and any resulting redness usually settles within a day or two from the procedure.

Determine The Right Treatment Plan for You
These are some of the most common and effective treatments for varicose veins, but there are additional methods tailored to individual cases. A thorough consultation with Dr Darryl Lim will help determine the best approach for your specific condition.
Why Choose Dr Darryl Lim
Dr Darryl Lim has years of experience caring for patients with complex vascular conditions. He previously served as Director of a high-volume vascular unit and later as a Service Chief at the SingHealth-Duke NUS Vascular Centre. Recognised as a vascular specialist by the Singapore Medical Council since 2015, he was also a Fellow of the Royal College of Surgeons of Edinburgh and the Academy of Medicine Singapore. Patients value his combination of expertise, compassion, and dedication to helping them achieve the best possible outcomes.
Dr Darryl has performed more than 3,000 interventional endovascular procedures to date. His approach allows patients to deal directly with him instead of a revolving team of doctors, from their first ultrasound to post-surgical consultations.
His expertise extends beyond varicose veins to include treatment of aortic aneurysms, peripheral vascular disease, and dialysis-access issues. This broad scope gives him a sharp eye for circulation problems that might otherwise be missed. Should other concerns arise, he promptly coordinates with your GP, endocrinologist, or cardiologist, ensuring that all your care providers stay informed and work together seamlessly.
See Dr Darryl for a Vein Assessment
Varicose veins often respond better when addressed early. If you’re noticing signs of vein issues, book an assessment with Dr Darryl Lim to better understand your condition and explore suitable next steps.

Insurance Claim Eligibility for Spider Vein Treatment
Spider vein treatment by itself is usually considered a cosmetic procedure and is not covered by most insurance providers. However, if your duplex scan reveals underlying venous reflux and you have related symptoms (such as leg pain, swelling, or heaviness), coverage for treatment may apply.
The amount covered may depend on your plan tier and rider. Most patients find that their share is limited to the MediSave portion or a modest co-insurance payment.
To check if your claim is eligible, follow these steps:
- Send our team at the clinic the details of your policy so that we can run the pre-authorisation process and tell you the approved amount before you commit.
- Touch base with your insurance agent and ask for confirmation of riders or co-insurance conditions.
- Check MediSave claims eligibility. The withdrawal limit is set by the MOH surgical table for the procedure to be performed, and can offset a part of the cost or even all of the bill in some cases.
If you do not have private insurance, speak with our team. We can walk you through the available options and craft an affordable treatment plan that still delivers the care you deserve.
FAQs on Spider Veins
Spider veins are generally harmless and mainly a cosmetic concern. Serious complications are uncommon, but if you notice swelling, pain, or other symptoms, it’s best to arrange a consultation with a healthcare professional to ensure there are no underlying conditions and to discuss treatment options early.
Generally, spider veins are treated with less invasive methods like injection sclerotherapy or radiofrequency treatment. Spider veins usually require a few sessions of sclerotherapy to resolve.
Varicose veins may additionally require more extensive treatment like mini-stab avulsions (for removal) depending on their extent and severity.
Because spider vein work is considered cosmetic, it is not typically covered by most insurances. For optimal results, Dr Lim usually combines injection sclerotherapy with VeinGogh® ohmic thermolysis in the same session.
If your duplex ultrasound scan shows significant reflux and you’re dealing with heaviness, swelling, or night-time calf cramps, fixing that leak moves from cosmetic to medical. At that point, most Integrated Shield Plans and Medisave can pick up a good share of the bill, easing the financial load. Speak with us for more information.
Yes. There is a possibility that new spider veins may develop over time even after successful treatment, particularly if underlying risk factors are not addressed. Risk of recurrence is usually around 5-10%.
This depends on the type of treatment you undergo. For minimally invasive treatments, most people can return to normal activities relatively quickly in a day or two. Vigorous exercise is usually not recommended till 2 weeks post-surgery. Traditional open surgical treatments may require a longer period for full recovery.

