
Many people think of varicose veins as a cosmetic issue- visible, bulging veins that affect appearance more than health. But varicose veins can do more than change how your legs look. When the underlying vein problem is left untreated, it can gradually damage the skin around the lower legs and ankles.
If you’ve noticed itching, dryness, eczema-like patches, brown discolouration, tight or thickened skin, or a wound that’s slow to heal near the ankle, these changes are often not random. They’re common signs of chronic venous insufficiency and deserve a proper assessment.
In this article, Dr Darryl Lim, a vascular and varicose vein specialist in Singapore, explains how varicose veins affect the skin, what to watch for early, and why treating the cause matters.
How varicose veins affect the skin
Varicose veins develop when one-way valves inside the leg veins fail. Normally, these valves help keep blood moving upwards towards the heart. When valves don’t close properly, blood can fall backwards (venous reflux) and pool in the lower legs.
That backward flow increases pressure inside the veins — this is chronic venous insufficiency (CVI). Over time, the elevated pressure doesn’t just affect the veins; it affects the surrounding skin and tissues.
When blood pools and pressure stays high:
- Oxygen delivery to the skin can drop
- Waste products accumulate
- Inflammation increases
- Fluid leaks into surrounding tissue
The result is skin that becomes gradually more fragile, more irritable, and slower to heal.
Early skin changes caused by varicose veins
Skin damage from vein disease usually develops slowly. Many people brush off early signs as “dry skin”, allergies, or ageing.
Persistent itching or irritation
This is one of the earliest clues. With venous pressure, inflammatory substances can leak into the skin and trigger itching. Scratching then makes the skin more likely to break, ooze, or get infected.
If the itch is concentrated around the lower leg or ankle and keeps coming back, it’s worth thinking about an underlying vein issue.
Dry, flaky, or sensitive skin
Inflammation and chronic venous pressure can impair the skin’s barrier. Moisturisers may help temporarily, but symptoms tend to recur if the underlying circulation issue isn’t addressed.
Redness or inflammation near the ankle
Chronic pooling can cause low-grade inflammation that looks like a persistent red patch or rash, often worse after standing.
These early changes are commonly grouped under venous eczema, also known as stasis dermatitis.

Skin Discoloration is a key warning sign
As venous disease progresses, skin discolouration becomes more obvious. This is the point where many patients start to worry (rightly).
Brown staining near the ankles
A very common description is: “brown stains on my ankles” or “my ankles look permanently dirty”.
This happens when red blood cells leak out of the veins and break down in the surrounding tissue. Iron-containing pigment (haemosiderin) remains in the skin, causing a brown or purplish appearance.
This isn’t surface staining. It reflects ongoing high internal venous pressure.

Bluish or purple changes
In some cases, reduced oxygen delivery and congestion can make the skin look bluish or purplish, especially after long periods of standing.
Discolouration usually means venous pressure has been elevated for a long time and shouldn’t be ignored.
Skin thickening and hardening (Lipodermatosclerosis)
One of the more serious forms of skin damage caused by varicose veins is lipodermatosclerosis.
This condition involves:
- Thickened, hardened skin
- Tightness around the lower leg
- Pain or tenderness
- A tapered or “inverted champagne bottle” appearance of the lower leg
This happens because chronic inflammation leads to scarring in the skin and the fat beneath it. At this stage, the skin becomes fragile and more prone to injury- even minor knocks can lead to breakdown.
CEAP classification: where skin changes fit in (C4/C5/C6)
In vein medicine, we often describe the severity of varicose vein disease using the CEAP clinical classification. It’s a helpful way to understand why skin changes matter because once the skin is involved, we’re no longer talking about “cosmetic veins”.
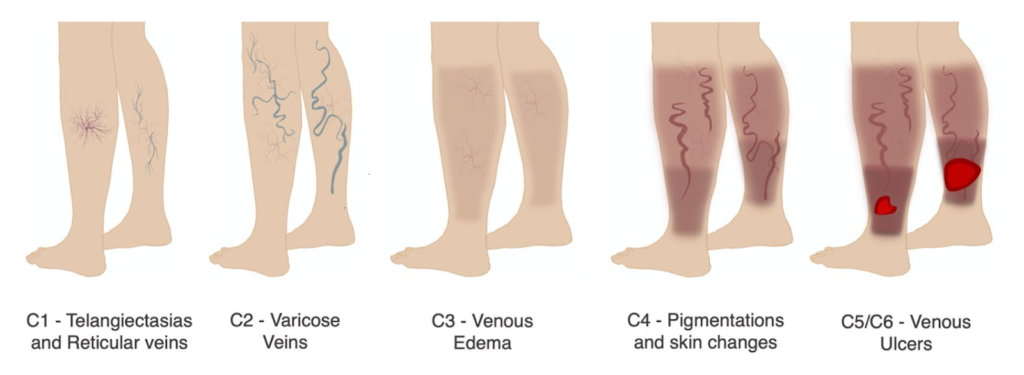
CEAP classification of chronic venous disease showing stages C1 telangiectasia, C2 varicose veins, C3 venous oedema, C4 skin pigmentation and changes, and C5/C6 venous ulcers.
Here’s the simplified progression:
- C1: Spider veins and reticular veins
- C2: Varicose veins
- C3: Venous oedema (persistent ankle/leg swelling)
- C4: Skin changes (eg. venous eczema, stasis dermatitis, brown pigmentation, or lipodermatosclerosis)
- C5: A healed venous ulcer
- C6: An active venous ulcer (open sore)
The key point is this: itching, eczema-like rash, brown ankle staining, and skin hardening often place you in C4 disease– a sign the condition has moved beyond appearance alone. At this stage, treating the underlying reflux becomes important to reduce the risk of progressing to ulcerative disease (C5/C6).
Can varicose veins cause open sores or ulcers?
Yes. Venous ulcers are one of the most serious complications of untreated venous insufficiency.


C5 Disease: healed venous ulcer C6 Disease: active venous ulcer
How venous ulcers form
Persistent high pressure in the veins reduces oxygen and nutrient delivery to the skin. Even a minor scratch or bump can fail to heal properly. Over time, this can develop into an open wound (most commonly near the inner ankle).
Venous ulcers:
- Heal slowly
- Can recur repeatedly
- Are prone to infection
- Significantly impact quality of life
Once ulcers develop, treatment becomes more complex- which is why it’s far better to catch and treat the problem earlier, when skin changes first appear.
Why skin damage means the disease Is progressing
Skin changes do not occur in isolation. They usually signal that venous insufficiency has moved beyond early-stage vein enlargement.
When skin damage is present, it often means:
- Venous pressure has been elevated for months or years.
- Valve failure is significant.
- Conservative measures alone may no longer be enough
At this stage, treating the skin while ignoring the reflux source rarely leads to lasting improvement. It’s like mopping up water without turning off the tap.
Common myths that delay treatment
“It’s just dry skin.”
If itching or dryness persists despite moisturisers (especially around the ankle), vein-related inflammation should be considered.
“It’s part of getting older.”
While aging increases vein disease risk, skin damage is not a normal part of aging. It often reflects a treatable circulation issue.
“I’ll deal with it if it gets worse.”
By the time ulcers appear, treatment becomes more difficult and recovery takes longer. Early care is usually simpler and more effective.
What it might be instead (and why assessment matters)
Not every rash or ankle discolouration is venous disease. Other conditions can look similar, such as:
- Fungal skin infection
- Contact dermatitis (e.g., footwear, creams, plasters)
- Cellulitis (skin infection)
- Arterial circulation problems (especially if there are ulcers or severe pain)
- Diabetes-related skin or wound issues
This is another reason not to self-diagnose. The pattern, location, and ultrasound findings guide the right treatment.
How varicose vein-related skin damage is diagnosed
A proper evaluation looks beyond what’s visible on the surface.
Duplex ultrasound
The key test is duplex ultrasound, which:
- Assesses vein valve function
- Identifies reflux (backward blood flow)
- Maps which veins are driving the pressure problem
Pinpointing the reflux source is critical. If you treat the wrong veins (or only what you can see), symptoms and skin problems often persist.
Can treating varicose veins improve skin damage?
In many cases, yes- especially when treatment occurs early.
By correcting the underlying venous reflux:
- Pressure in the legs decreases
- Inflammation is reduced.
- Skin receives better oxygen and nutrient supply
- Healing improves
Patients often notice:
- Less itching and irritation
- Gradual lightening of discoloration
- Reduced swelling
- Improved skin texture
That said, long-standing pigmentation and advanced scarring may not fully reverse. This is why early treatment is so important.
Need an expert vascular opinion for your Varicose Veins?
Book an appointment with Dr. Darryl Lim today and get a personalized treatment plan.

Modern treatments that address the root cause
Today’s vein treatments are minimally invasive, outpatient procedures designed to close or remove diseased veins so circulation reroutes through your healthier veins.
Depending on ultrasound findings, options may include:
- Endovenous Radiofrequency Ablation (RFA)
- Medical adhesive closure (VenaSeal)
- Ultrasound-guided Sclerotherapy
- Microphlebectomy for surface varicose veins
These are usually day procedures with minimal downtime. The aim is to lower venous pressure in the legs and stop the skin changes from progressing, not purely for cosmetic improvement.
How to Protect Your Skin While Managing Vein Disease
While medical treatment addresses the cause, supportive measures can help protect fragile skin:
- Moisturize regularly with gentle, fragrance-free products.
- Avoid scratching irritated areas.
- Elevate your legs daily to reduce swelling.
- Wear compression stockings if recommended.
- Protect the skin from injury, especially near the ankles.
If there is an open wound, it’s important to get proper assessment (and in some cases, arterial circulation checks) before using strong compression.
When to Seek Professional Care
You should seek evaluation if you notice:
- Persistent itching or eczema-like changes near the ankles
- Brown, purple, or dark skin discoloration
- Tight, hardened skin on the lower legs
- Recurrent swelling
- Slow-healing wounds or open sores
Also seek urgent review if you develop spreading redness, warmth, increasing pain, fever, or discharge as these signs may suggest infection.
The Bottom Line
Varicose veins can cause skin damage, and it’s often a sign of progressing venous disease rather than a superficial skin problem.
Itching, discolouration, thickening, and ulcers happen when prolonged venous pressure damages the surrounding tissue. Treating the skin alone is rarely enough. Addressing the underlying reflux is what protects the skin and prevents serious complications.
Early diagnosis and modern treatment can reduce symptoms, support healing, and help prevent ulcers.
Frequently Asked Questions
Can spider veins also cause skin damage?
Spider veins alone usually do not cause significant skin damage. However, they can coexist with deeper venous insufficiency, which can.
Is skin discoloration from varicose veins permanent?
Early discoloration may improve after treatment. Long-standing pigmentation may fade slowly or remain partially permanent.
Do compression stockings prevent skin damage?
Compression can reduce pressure and swelling, helping protect the skin, but it does not correct faulty vein valves.
When are venous ulcers most likely to occur?
Ulcers are more likely when venous insufficiency has been long-standing and untreated, especially when there is ankle swelling and skin discolouration.

















