If you’ve been dealing with a stubborn wound that just won’t seem to heal, you might feel frustrated, anxious, or even a bit uncertain. Traditional methods—keeping the area clean, changing dressings frequently, and waiting it out—don’t always bring the results you expect.
There is another approach that many doctors, including vascular surgeons such as Dr. Darryl Lim, rely on. Known as negative pressure wound therapy, this method applies gentle, controlled suction to encourage faster, more effective healing. Although it may sound a bit high-tech at first, it can often make a tangible difference for patients stuck in a slow, difficult healing process.

How Negative Pressure Wound Therapy Works
At its core, negative pressure wound therapy involves using a specialized dressing and a small vacuum device to create a carefully calibrated suction over the wound. Rather than simply covering the wound and hoping for the best, this technique helps remove excess fluid and debris. It draws the wound edges closer together and supports healthier blood flow, allowing the body to focus on building fresh tissue.
When the environment around a wound is carefully managed, the body’s natural healing process can move forward more efficiently.
Why Some Wounds Need Extra Help
Certain wounds, such as diabetic ulcers, pressure sores, or those that fail to close after surgery, benefit from more than just basic bandages. Poor circulation, underlying infections, or other medical conditions can slow recovery. You might find that a wound stays open for weeks, leaking fluid and feeling tender.
Negative pressure wound therapy tackles these issues directly by gently removing fluid, reducing swelling, and cutting down on bacterial growth. Freed from these barriers, fresh blood reaches the area more easily, bringing vital oxygen and nutrients. Over time, this can significantly improve the wound’s condition and help it close.

What to Expect from Treatment
When you begin negative pressure wound therapy, a wound care specialist or nurse places a foam or gauze dressing into the wound. A clear, protective film creates a seal on top. A thin tube connects this setup to a small vacuum device that provides a constant, low-level suction. Although the sensation may feel unusual at first, most patients grow accustomed to it. The device’s gentle hum can become part of your normal routine, and it’s often encouraging to see the wound gradually improve in appearance and comfort.
Living with a Negative Pressure Wound Therapy Device
Modern machines are designed with patient comfort in mind. Some units are compact and portable, allowing you to move around your home, take short walks, or continue many of your usual daily activities. If your wound isn’t severely complicated, you may even be able to manage therapy at home with occasional guidance from a wound care nurse or vendor. They can advise on how often to change the dressing, how to keep the device clean, and what signs to watch for, ensuring you remain actively involved in your own care.
Advanced Techniques: Instillation Therapy
For more complex wounds or those producing large amounts of fluid, some variations of negative pressure wound therapy include instillation. In these cases, a specialized solution is introduced into the dressing and then removed by the vacuum. This dual-action technique can be particularly effective for difficult wounds, cleansing away bacteria and stubborn debris. While it may require closer oversight—often in a clinic or hospital setting—it can be a valuable tool for patients who’ve had trouble progressing with standard therapies.
Addressing Common Concerns
As with any treatment, negative pressure wound therapy isn’t without potential discomfort. Some patients report mild pain or sensitivity during the first few days, especially while adapting to the dressing and suction. Healthcare providers can help manage this with pain relief strategies or by fine-tuning the device’s settings. There’s also some maintenance involved: dressings need routine changes, and the device must be kept clean. In certain cases, your healthcare team may recommend limiting particular activities until healing is well underway. Although these steps require patience and diligence, many patients find the payoff – in terms of reduced pain, better wound appearance, and steady progress – well worth it.
How Long Does Therapy Last?
The duration of treatment varies. Some patients notice improvements within 1-2 weeks, while others with deeper or more complicated wounds may need therapy for a longer period. Your wound care specialist will monitor your progress, watching as the tissue responds and the wound edges draw closer. Over time, they’ll determine when it’s appropriate to transition to a different form of care or possibly stop using negative pressure altogether. The goal is always to find the best route to reliable, lasting healing.
Poorly Healing Wound?
Chronic wounds can be frustrating and slow to heal. Advanced therapies are available to speed recovery and reduce the risk of infection.

Steady Progress, Informed Decisions
As technology evolves, negative pressure wound therapy machines are becoming quieter, simpler to operate, and far more patient-friendly. Treatments that once meant lengthy hospital stays and multiple visits can now be easier to manage, giving you more control over your healing process. By speeding up wound closure and lowering the chances of infection, this therapy often means fewer invasive procedures and, ultimately, a more cost-effective path toward better health.
If you’re curious about whether negative pressure wound therapy is the right choice for you, don’t hesitate to open up to your healthcare team. Bring your questions, your concerns, and your hopes for a smoother recovery. With the guidance of a skilled professional, you’ll have the confidence to move forward.
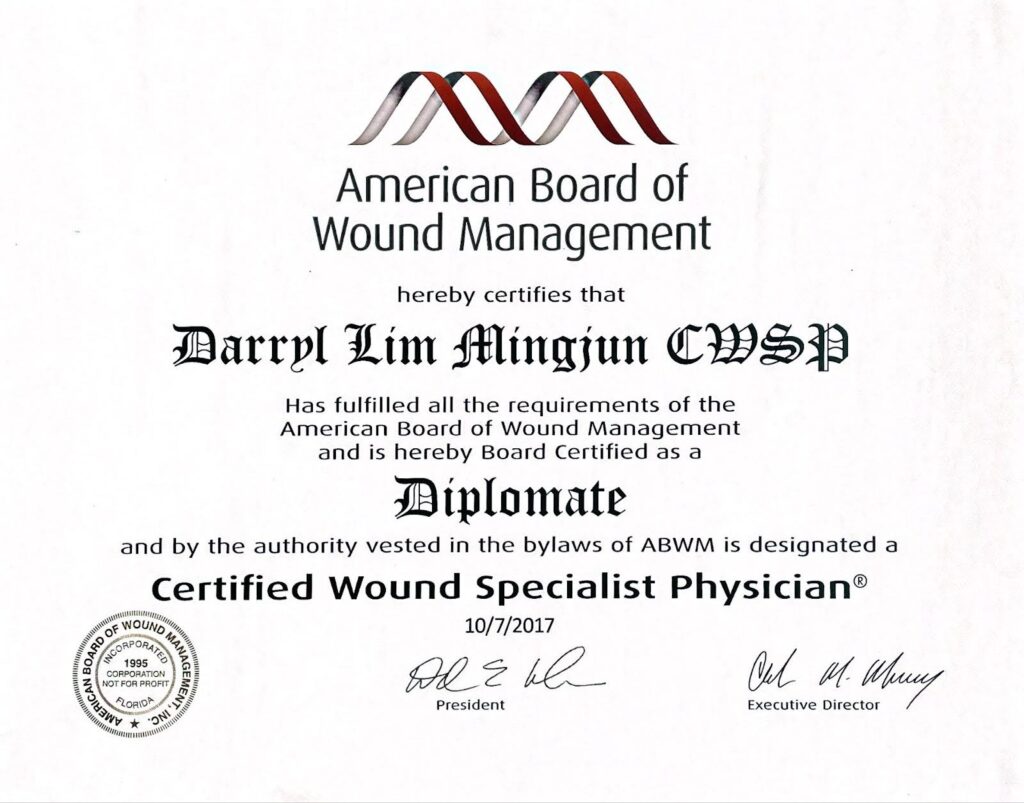
Dr. Darryl Lim, certified by the American Board of Wound Management as a Wound Specialist Physician (CWSP), takes a sincere, patient-centered approach to managing complex and challenging wounds. By pairing evidence-based therapies with genuine compassion, he aims to promote more efficient healing and help prevent future setbacks. Under his care, you’ll find not only relief and reassurance, but also the support you need to restore comfort, confidence, and a sense of normalcy in your everyday life.

















