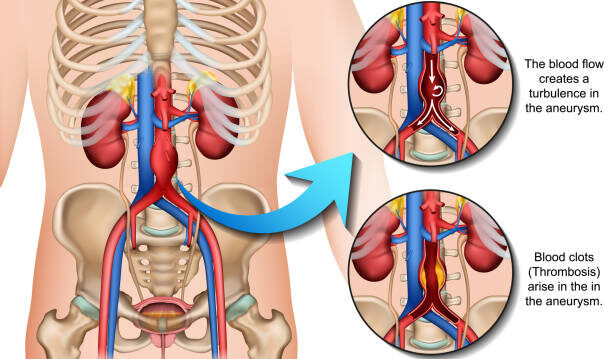
Your aorta is the body’s main “highway”, transporting blood pumped out from the heart to the rest of the body. An aortic aneurysm is a weak spot on that highway that balloons out- most often in the abdomen (AAA). It’s usually silent, but if it bursts, it can cause life-threatening internal bleeding. The aim is to find it early, keep an eye on it, and fix it if it gets too big.

If you’re in Singapore and wondering whether you should be screened, you can arrange for an assessment and screening with Dr Darryl Lim, Vascular & Endovascular Surgeon.
Meet the Aorta (and the “bulge”)

Picture your aorta like a garden hose running from your heart through your chest and tummy, delivering blood everywhere. If a section weakens, it gradually balloons out- that’s what an aneurysm is.
Over time, that weak spot can grow and thin, raising the risk of rupture — a medical emergency. That’s why early detection and monitoring are key to preventing serious complications.
Types you’ll hear about:
- AAA (Abdominal Aortic Aneurysm): the common one, in the tummy.
- TAA (Thoracic Aortic Aneurysm): higher up, in the chest.
- Thoracoabdominal: spans both regions.
We’ll focus on AAA because that’s what screening usually targets.
Why it matters
Most aneurysms cause no symptoms for years. The risk of rupture rises as they grow. A rupture is a medical emergency with a high risk of death. The good news is that with monitoring and timely repair, outcomes are often very good.
How common are Abdominal Aortic Aneurysms (AAA) ?
Abdominal aortic aneurysms aren’t common in the general population, but they’re not rare either—especially as we age. Globally, about 1% of people aged 30–79 are living with an AAA, with men affected far more often than women (~1.46% vs ~0.39%).
In Asia including Singapore, the overall prevalence sits around ~1.3%, but climbs to roughly 2.5–4% in higher-risk groups (typically older men above 60 with cardiovascular risk factors or a smoking history).
So while Singapore’s rates are lower than many Western countries, if you (or a loved one) fit that higher-risk profile, it’s worth a simple chat about one-off ultrasound screening to put your mind at ease.
Why do aneurysms form?
In many people, it’s simply due to “wear and tear” of the body mixed with a few nudges from risk factors.
As we age, the aortic wall naturally stiffens and weakens. Smoking is the single biggest culprit, as it directly damages the vessel lining. High blood pressure and atherosclerosis add constant strain and inflammation, encourage a weak spot to balloon over time.
Some of us are also born with a thinner safety margin because of family history or genetic conditions that affect connective tissue in the arteries, and men are affected more often than women.
Bottom line: Cut what you can- especially stop smoking and control your blood pressure. Once this is done, you meaningfully lower the risk of an aneurysm developing or growing.
Will I feel it if I have a Aortic Aneurysm?
Often, no. That’s the trap.
Possible clues (usually when larger): a deep ache in the back or tummy, or a pulsating feeling in the abdomen.
Emergency red flags: sudden, severe tummy or back pain, collapse, or fainting- call for help immediately.
How do we test for Abdominal Aortic Aneurysms (AAA)?
- Ultrasound of the abdomen (screening): quick, painless, radiation-free.
- CT/MRI scan: used when we need more detail, and for surgical planning.
If you’re male and 65–75 and have ever smoked, most international guidelines recommend a one-off ultrasound to check your abdominal aorta.
If you’ve never smoked but are in that age band, it’s still worth a chat with your doctor about an ultrasound screen- especially if you have a family history of aneurysm or heart-health risks. In Singapore, screening isn’t automatic, so your vascular surgeon can arrange it quickly if you’re a suitable candidate.
What happens if I have one?
It really comes down to size and how quickly it’s growing. Small aneurysms usually don’t need an operation; we keep a close eye on them with regular scans and tighten up the risk factors- stop smoking, get blood pressure and cholesterol under control, and stay active. If the aneurysm is large or starts growing faster, surgical repair is the safer path. That’s typically either:
Endovascular repair (EVAR): a minimally invasive option where a stent-graft is placed through small cuts at the groin. Post-op recovery is usually much quicker.
Open repair: a durable surgical graft through an abdominal incision- chosen when EVAR isn’t ideal or by preference.
Your vascular surgeon will talk you through the pros and cons of each, then recommend the approach that best fits your anatomy, health, and goals.
Take-home message
If you’re a man over 65 and have ever smoked, it’s sensible to ask about a one-off ultrasound to check your abdominal aorta. If aneurysms run in the family, bring it up with your doctor earlier. Don’t wait for symptoms- most people feel nothing until it’s urgent.
When treated electively at the right time, surgical outcomes are good. If you’d like a personalised screening or a second opinion, you can book a consult with Dr Darryl Lim; he’ll review your risks, arrange the appropriate scan, and talk you through the options available.
FAQ
Is an aneurysm the same as a blocked artery?
No- an aneurysm is a ballooning of the vessel, not a blockage (though both can coexist).
Can it shrink by itself?
Not typically. We monitor, modify risks, and repair if it reaches the threshold.
What size needs surgery?
Rules vary by sex and anatomy, but many centres consider repair once an AAA is around 5–5.5 cm or if it’s growing quickly.
Can lifestyle changes help?
Yes. Stopping smoking is the single best step. Also: manage blood pressure, cholesterol, weight, and activity.