In Part 1 of this series, we explored what Pelvic Congestion Syndrome (PCS) is, why it happens, and how it’s diagnosed- particularly in women struggling with chronic pelvic pain that often goes unexplained. In this follow-up, we turn our attention to treatment. The good news is that PCS is highly treatable, especially with today’s minimally invasive techniques.
Dr. Darryl Lim, a vascular and endovascular surgeon in Singapore, specialises in advanced endovascular procedures that avoid the need for large incisions or open surgery. Treatment plans are tailored to each patient’s needs, taking into account symptom severity, reproductive goals, and the specific vein abnormalities present. From conservative approaches to targeted interventions like embolisation and stenting, women now have a range of effective options to achieve lasting relief.
In general, treatment of PCS falls into a few categories:
Conservative Management
For mild cases or as an initial approach, conservative measures can help manage symptoms. This includes pain relief medications (NSAIDs like ibuprofen or acetaminophen) to reduce pelvic ache, lifestyle changes such as avoiding prolonged standing/heavy lifting (to minimize pelvic vein pressure), taking breaks to elevate legs or lie down during the day, doing regular low-impact exercise (walking, swimming, yoga) to improve circulation, and weight management (to reduce pressure on pelvic veins).
Some women may also benefit from wearing compression garments (if PCS results in varicose veins in the thighs or legs)- for example, graduated compression stockings (thigh-high) can aid leg vein blood return. While these measures don’t fix the underlying vein reflux, they can provide partial symptomatic relief and improve quality of life.
Medical Therapy (Hormonal)
Hormonal medications can be used to alleviate PCS symptoms, particularly if there are no plans for pregnancy in the near term. Because estrogen seems to contribute to vein dilation, drugs that suppress ovarian estrogen production can lead to “shrinkage” and decreased congestion of the pelvic varices.
Examples include medroxyprogesterone acetate or GnRH agonists, which induce a temporary menopause-like state with low estrogen. Birth control pills are sometimes used to blunt hormonal fluctuations. These therapies often help reduce pelvic vein engorgement and pain. However, do note that hormonal treatment is usually a short-term or adjunct solution- symptoms often recur when medication is stopped, and long-term use can carry side effects. Dr. Darryl Lim works closely with gynecologists when using this option, to ensure the therapy aligns with the patient’s reproductive plans and health profile.
Minimally Invasive Endovascular Treatment
These endovascular treatments address the root cause by closing off the problematic veins so blood reroutes through healthy pathways. Dr. Lim typically performs these procedures under light sedation and local anesthesia. The mainstay interventions for PCS include ovarian/pelvic vein embolization and, if needed, venous stenting for any compression syndromes.
(I) Ovarian and Pelvic Vein Embolization
This is the first-line definitive treatment for PCS. Embolization is a “keyhole” procedure that involves sealing off the refluxing ovarian/pelvic veins from within. Through a tiny 2-3mm skin incision (typically at the groin or neck), a catheter is navigated into the dilated ovarian veins under X-ray guidance. Dr. Lim will then perform a venogram to identify the diseased veins and deliver embolic agents to block them. Embolic agents may include tiny metallic coils and/or a sclerosing substance (a medical glue or irritant foam) injected through the catheter. The coils act like plugs that induce clotting, while the sclerosant irritates the vein lining to scar it closed. By closing off these faulty veins, blood can no longer pool in the pelvis and is rerouted to healthier veins. Without the high-pressure from venous reflux, there should be significant improvement in the pelvic pain.
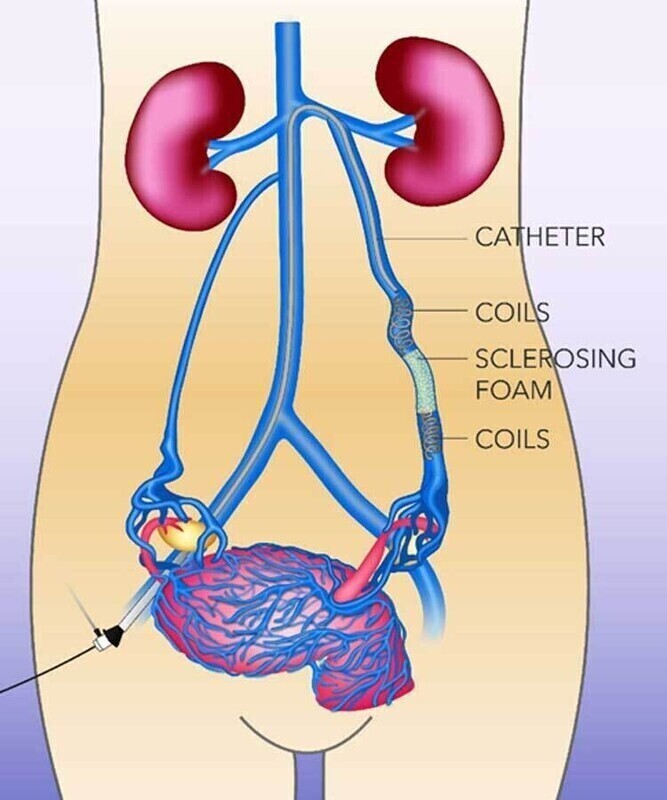
During ovarian vein embolization, a catheter is guided to the ovarian veins and coils (plus sometimes a sclerosing foam) are placed to seal the vein.
The procedure itself usually takes around an hour, and patients can either go home the same or next day. Studies show a high success rate for ovarian vein embolization- around 80% of patients have significant pain relief after the procedure. Some patients report improvement within days, with full benefits realized over a few weeks as the congested veins completely close and shrink. Notably, embolization preserves the ovaries and uterus, so future fertility is retained; women can still become pregnant afterward, although it’s usually recommended to wait a few months post-procedure before trying to conceive.
In some cases, embolization is combined with pelvic variceal sclerotherapy – if there are multiple smaller varicose vein networks in the pelvis or visible vulvar varices, the doctor can inject sclerosant directly into those as well for a thorough treatment. Overall, ovarian/pelvic vein embolization is a safe and effective solution that directly targets the cause of PCS.
(II) Iliac Vein Stenting (for May-Thurner Syndrome)
If diagnostic imaging reveals an underlying May-Thurner syndrome (i.e. compression of the iliac vein leading to venous hypertension)- this can be a contributory cause to the pelvic congestion. In such cases, concomitant treatment of this compression is important.
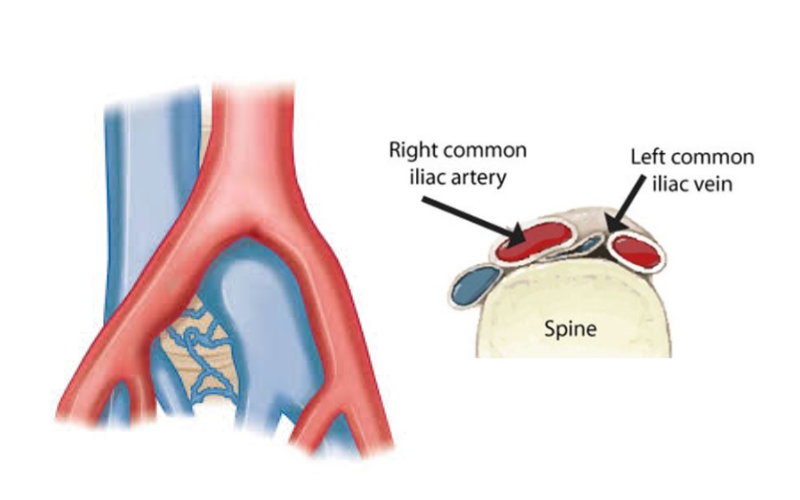
Iliac vein stenting involves placing a small metal mesh stent in the compressed segment of the vein to prop it open. This can be done in the same sitting as the embolization procedure. By relieving the iliac vein blockage, normal blood outflow from the legs and pelvis is restored, which in turn lowers the pressure in the pelvic veins downstream. Do note that not every PCS patient will require a stent- only those with a significant venous compression documented on imaging. Dr. Lim will only proceed with stenting if indicated, but having the capability to stent means we can comprehensively treat patients who have both Pelvic Congestion Syndrome and May-Thurner Syndrome.
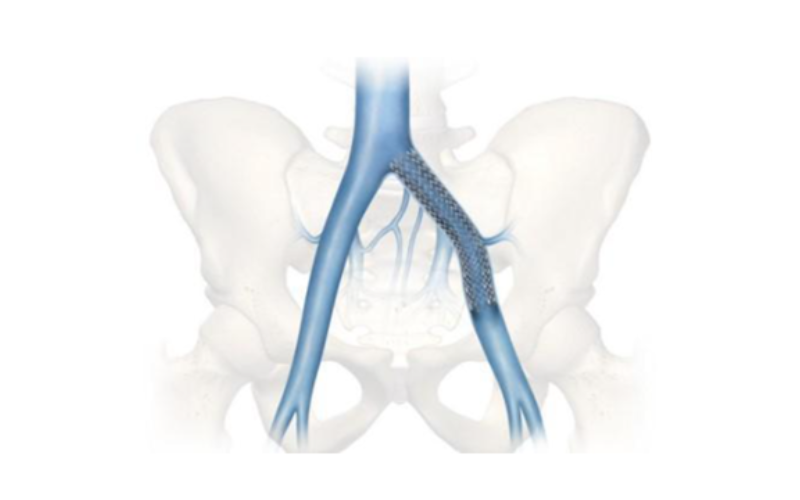
Doing both procedures in one sitting ensures the root cause of the congestion is fully resolved. Iliac vein stenting has high technical success in alleviating the venous narrowing, and when combined with embolization, it can significantly improve outcomes.
(III) Renal Vein Stenting (for Nutcracker Syndrome)
In some patients- especially those with symptoms on the left side (blood in urine, left flank pain)- Nutcracker syndrome may be the culprit. This is when the left renal vein is compressed, which in turn causes left ovarian vein reflux and varicose veins in the pelvis. For confirmed Nutcracker syndrome causing significant symptoms, renal vein stenting is a potential treatment option.
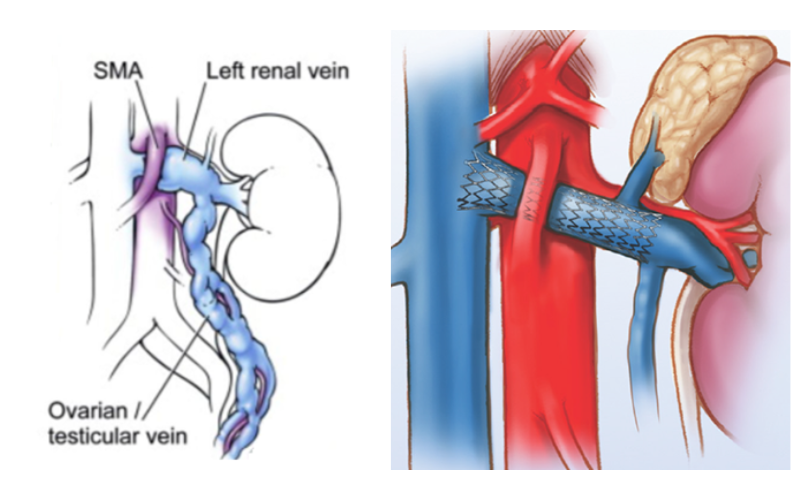
In this procedure, a stent is placed in the left renal vein to relieve the pinched segment and restore normal blood flow from the kidney. By doing so, the backpressure into the ovarian vein is reduced, which can alleviate pelvic congestion. A common approach is to embolize the ovarian vein and stent the renal vein if the patient has Nutcracker-related pelvic congestion. Stenting the renal vein is also minimally invasive, done via a keyhole technique similar to iliac stenting.
Surgical Option
In the vast majority of cases, the minimally invasive treatments discussed above are suffice to relieve PCS. Surgery is often a last resort- for example in instances where symptoms are refractory. Surgical options include ovarian vein ligation (tying off or removing the ovarian veins through an abdominal incision), or left renal/gonadal vein transposition (in the case of Nutcracker Syndrome). Open surgeries are typically associated with a longer post-operative recovery period. Fortunately, such invasive measures are seldom required nowadays, given the high success rates of keyhole techniques.
Treatment Outcomes and Recovery
Most women experience significant improvement in symptoms after appropriate therapy. Ovarian vein embolization and related endovascular procedures have reported success rates in medical literature of about 70–85% in terms of symptom relief.
One major advantage of the minimally invasive treatments is the quick recovery time. Unlike open surgery, these procedures don’t involve large incisions, and are essentially “scarless”. Most patients can go home the same or next day after an embolization or stenting procedure. After the treatment, it’s normal to have mild soreness at the catheter entry site (often the groin or neck) or a transient deep ache in the pelvis for a few days. This post-procedure pain is usually mild and well-managed with painkillers and rest. There may also be some low-grade fever or backache for a short time as the veins occlude – a minor inflammatory response. Doctors term this the “post-embolization syndrome,” but it is typically very manageable.
Patients are generally advised to take it easy for a couple of days. Light activities can often be resumed within 1–2 days, and most women are back to their normal routine within a week. Heavy exercise or lifting may be restricted for about 1-2 weeks to allow the veins to heal. Dr. Lim provides individualized guidance on activity resumption and any medications (for example, if a stent is placed, you may take blood thinners temporarily as mentioned). Follow-up scans are scheduled to monitor the progress of the closed veins.
Symptom relief is not always immediate, but many women start noticing improvement in pelvic pain within days to a few weeks after embolization. Full relief can take up to 3 months as the varicose veins gradually shrink and the pelvic circulation reroutes. Patience is key – the outcome is often very rewarding after those initial weeks. In successful cases, women report being able to stand or exercise longer without pain, and an end to the daily ache that was limiting their life.
Of course, individual results vary. A small subset of patients may experience only partial relief or recurrence of symptoms down the line. If pelvic pain persists despite an initially successful procedure, further evaluation will be done to investigate other pain sources or any residual veins that might need treatment. It’s also worth noting that if a woman becomes pregnant after a PCS treatment, some pelvic vein changes could potentially recur due to the pregnancy’s circulatory effects. However, having treated the major reflux beforehand still puts her in a much better position, and many women who have had embolization go on to have healthy, relatively comfortable pregnancies.
When to Seek Help (Getting a Diagnosis)
Chronic pelvic pain should never be dismissed as “in your head” or something you just have to live with. If you have had pelvic pain for more than 6 months and especially if you notice the characteristic patterns we discussed (worse with standing, after intercourse, around menstrual periods; presence of varicose veins, etc.), it’s important to seek a thorough evaluation. Start by talking to your primary doctor or gynecologist about your symptoms. In Singapore, many gynecologists are aware of pelvic congestion syndrome as a possible cause of unexplained pelvic pain (although awareness is still not universal). You may need to advocate for yourself and ask, “Could it be a vein issue?” If you have visible vulvar or thigh varicosities along with pelvic pain, be sure to point them out, as not all doctors will immediately connect those dots.
Generally, an OBGYN will first investigate more common causes of pelvic pain (like endometriosis or ovarian cysts). If those are ruled out and especially if you have risk factors for PCS (multiple children, known varicose veins, etc.), you should request or be referred for a pelvic vein evaluation. This might involve seeing a vascular specialist.
Do not hesitate to seek a second opinion if you feel your concerns are not being fully addressed. Many women with PCS see multiple doctors over years before getting the correct diagnosis. If you recognize that your symptoms match what’s described, consider consulting a clinic that focuses on venous disorders.
Insurance and Subsidy Considerations in Singapore
Treatment for pelvic congestion syndrome in Singapore can be accessible and affordable, especially with insurance or medisave support. Here are some key points regarding costs and coverage:
- Insurance Coverage: Dr. Darryl Lim is on the panel of many major local insurance providers, and his clinic follows the Ministry of Health (MOH) fee benchmark guidelines. This means if you have a private health insurance or integrated shield plan, there’s a good chance that consultations and procedures for PCS will be covered (fully or partially) as medically necessary treatments. It’s always wise to check with your insurer, but ovarian vein embolization and related interventions are recognized treatments- most insurers cover them under specialist care for varicose veins or vascular conditions. If Dr. Lim is a panel specialist on your plan, your out-of-pocket costs will be lower; even if not, you can often claim reimbursement with the clinic’s help in documentation. Always obtain a Letter of Guarantee (LOG) from your insurer before a procedure if possible, to smooth the claims process.
- MediSave: For Singapore citizens and PRs, MediSave can typically be used for inpatient or day-surgery procedures, including those for vascular conditions. Dr. Lim is Medisave-accredited, meaning you can tap your MediSave savings to partially offser the bill for eligible treatments.
- Miscellaneous: Always discuss with the clinic’s billing staff about your coverage. Even if your doctor is not on the insurer’s direct panel, the clinic can assist with LOG requests to check your reimbursement coverage. There are also MOH fee benchmarks available publicly (for example, code SI703O covers ovarian vein embolization for PCS) that show typical price ranges for a range of procedures- useful if you want to gauge costs.
Need Expert Vascular Care?
Book an appointment with Dr. Darryl Lim today and get a personalized treatment plan for your vascular health.

Conclusion
Living with chronic pelvic pain can feel isolating- but Pelvic Congestion Syndrome is a treatable condition, and with the right care, most patients can regain control of their comfort and quality of life. The key is timely diagnosis, appropriate intervention, and support from a multidisciplinary team that understands this often-overlooked condition. If your symptoms match what’s been described, don’t hesitate to take the next and reach out to us.
Frequently Asked Questions about Pelvic Congestion Syndrome (PCS) Symptoms and Diagnosis
Q: What treatments are available for PCS?
A: Conservative options include painkillers, hormonal therapy (e.g. medroxyprogesterone or GnRH agonists), and lifestyle changes. The most effective treatment is ovarian vein embolisation, a minimally invasive procedure that blocks off the problematic veins. In certain cases, vein stenting or surgery may be needed.
Q: How long is the recovery after embolisation?
A: Most patients walk the same day. Light activities resume in 1–2 days, with full recovery in about a week. Mild pelvic cramps may occur. Symptom relief typically improves over 4–12 weeks.
Q: Does PCS affect fertility or pregnancy?
A: PCS doesn’t usually prevent pregnancy. Some women may conceive more easily after treatment. Embolisation preserves fertility, but it’s best to wait a few months post-procedure before trying to conceive.
Q: Can men have pelvic congestion syndrome?
A: No. PCS affects women due to their pelvic vein anatomy. Men can have varicoceles, which are similar but limited to the scrotum.
Q: Is treatment for PCS covered by insurance or MediSave in Singapore?
A: Yes. Most Integrated Shield Plans and MediSave cover PCS treatments like embolisation if medically necessary. It’s best to check with your clinic’s insurance coordinator for exact coverage.
Q: Can PCS come back after treatment?
A: Recurrence is rare but possible. New veins may enlarge or previously treated veins may reopen. Repeat embolisation can help if needed, and lifestyle measures may reduce the risk of recurrence.
Q: Where can I get treatment for PCS in Singapore?
A: PCS is typically treated by vascular surgeons. A referral from your OBGYN is often helpful to start the process.

















