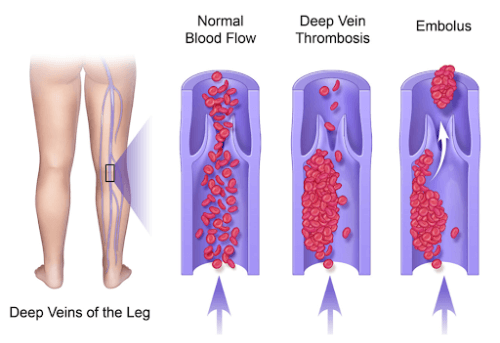
Deep Venous Thrombosis (DVT) is a condition where a blood clot forms in the deep veins of the body, most commonly in the legs. When a thrombus (clot) develops in a deep vein, it can partially or completely block blood flow, causing pain and swelling in the affected limb.
DVT is a serious medical condition because if the clot dislodges and travels through the bloodstream, it can lodge in the lungs as a pulmonary embolism (PE) – a life-threatening complication. Prompt diagnosis and treatment of DVT are crucial to prevent such dangerous outcomes and to reduce the risk of long-term complications.
Causes and Risk Factors of DVT
DVT usually occurs due to a combination of factors that affect how blood flows or clots. Common causes and risk factors include situations that slow down circulation or make the blood more prone to clotting:

- Immobility or prolonged sitting: Long periods of inactivity – for example, extended bed rest after surgery or sitting through a long-haul flight – can slow blood flow in the legs. This sluggish circulation can lead to clot formation.
- Recent surgery or injury: Surgery (especially orthopaedic or major surgeries) as well as physical trauma can damage blood vessels and trigger changes in the body that make clots more likely. Hospital stays after surgery, where patients are often less mobile, further increase the risk. This is why DVT prevention measures like compression stockings and early mobilisation are so important during recovery.
- Inherited clotting disorders: Some people have genetic conditions that make their blood clot more easily. A family or personal history of DVT or pulmonary embolism also increases your risk.
- Pregnancy and post-partum period: During pregnancy, increased pressure in the pelvic veins and changes in blood coagulability raise the risk of DVT. This risk can persist for several weeks after childbirth.
- Age over 40: While DVT can affect people of any age, the risk increases after age 40. Older adults often have more risk factors such as reduced mobility or underlying health issues.
- Overweight or obesity: Excess body weight adds pressure on the veins in the pelvis and legs, which can impair circulation and contribute to clot formation.
- Smoking: Tobacco use can affect blood flow and clotting mechanisms, making clots more likely to form.
- Hormonal factors: Birth control pills or hormone replacement therapy (HRT) can slightly increase the tendency of blood to clot. This is why doctors carefully evaluate DVT risk when prescribing these medications.
- Chronic medical conditions: Certain illnesses like cancer (and its treatments such as chemotherapy) and autoimmune diseases (e.g. lupus or inflammatory bowel disease) are associated with a higher risk of DVT. Cancer can increase clotting factors in the blood, and treatments or prolonged illness can reduce mobility, compounding the risk.
- Varicose veins: Significant varicose veins reflect chronic vein issues and can contribute to sluggish blood flow in the legs, which may elevate DVT risk.
- Central vein catheters: Having a central venous catheter or pacemaker in a large vein can irritate the vessel and become a focus for clot formation.
It’s important to note that DVT often arises from a combination of these factors. For instance, an older patient who is slightly overweight and undergoes a long airplane journey has multiple compounding risks.
In Singapore, where long flights are common and lifestyles can be sedentary for office workers, being aware of DVT risk factors is especially important. If you have one or more risk factors, taking preventive measures (like staying active, hydrated, or wearing compression stockings when appropriate) can significantly lower your chances of developing DVT.
Symptoms and Warning Signs
Recognizing the symptoms of DVT early is vital, as prompt medical attention can prevent serious complications. However, it’s also possible for DVT to cause very mild symptoms or even no noticeable signs in some cases. Up to one-third of people with DVT may not realize they have a clot until it causes a more severe issue. Common symptoms to watch for include:
- Leg Swelling: Swelling in one leg – typically starting in the calf and sometimes extending up to the thigh – is one of the most common signs of DVT. It often develops suddenly, and the affected leg may appear noticeably larger or tighter than the other. In some cases, the swelling can feel firm or tender to the touch.
- Leg Pain or Tenderness: DVT pain often starts in the calf and can feel like a cramp or a throbbing ache. The pain may worsen when standing or walking and improve with rest. The area might be tender to the touch, making it painful to press on the calf.
- Warmth and Redness: The skin over the affected area can become warm to the touch, and you might see redness or a darker color change on that leg. On lighter skin tones, a DVT can cause visible redness; on darker skin, it may appear as a deeper hue or simply feel warm and swollen.

- Visible Veins: Sometimes the veins near the surface of the skin become more prominent or swollen (sometimes described as “ropes”) in the affected leg due to the backed-up blood.
- Heaviness or Fatigue in the Leg: Some patients describe a heavy, tired feeling in the affected limb, or a sense that something isn’t right even before obvious swelling appears.
What About Arm DVT?
Though less common, DVT can also occur in the arms, particularly in people with IV lines, pacemakers, or thoracic outlet compression. Symptoms include arm swelling, pain, or a bluish discolouration of the hand or fingers.
It is critical to seek immediate medical attention if you have symptoms of DVT – especially if they are accompanied by chest discomfort or breathing difficulty. Signs that a clot may have travelled to your lungs (causing a Pulmonary Embolism) include sudden shortness of breath, chest pain (especially if it worsens when taking a deep breath), dizziness or fainting, or coughing up blood-tinged sputum. A pulmonary embolism can be life-threatening, so treat these symptoms as an emergency.
In essence, if you suspect DVT, do not ignore it. It’s always safer to have a doctor evaluate your symptoms promptly.
Diagnosis of DVT
Diagnosing deep vein thrombosis quickly and accurately is a priority. At our clinic, we provide on-site duplex ultrasound scanning to evaluate for DVT, which means you can get tested and results without delay. A duplex venous ultrasound is the first-line diagnostic test for DVT. It is a painless, non-invasive scan that uses sound waves to visualize the flow of blood in your veins. During the ultrasound, the sonographer will apply gentle pressure with the probe on your leg; if a vein does not compress under pressure, it suggests a clot may be present preventing the vein from collapsing as it normally would. In addition to diagnosing the presence of clot, the scan can help locate its position and extent.

Diagnosing deep vein thrombosis quickly and accurately is a priority. At our clinic, we provide on-site duplex ultrasound scanning to evaluate for DVT, which means you can get tested and results without delay. A duplex venous ultrasound is the first-line diagnostic test for DVT. It is a painless, non-invasive scan that uses sound waves to visualize the flow of blood in your veins. During the ultrasound, the sonographer will apply gentle pressure with the probe on your leg; if a vein does not compress under pressure, it suggests a clot may be present preventing the vein from collapsing as it normally would. In addition to diagnosing the presence of clot, the scan can help locate its position and extent.
In most cases, ultrasound is sufficient for diagnosis. However, depending on the situation, additional tests might be used:
- D-dimer blood test: This blood test detects a substance released by blood clots. A normal D-dimer test can make DVT less likely, whereas an elevated D-dimer (especially in a high-risk patient) might prompt further imaging. This test is more often used in the ER or for screening, and by itself it’s not confirmatory, but it can be a useful piece of the puzzle.
- CT Scan: If a DVT is suspected in a location not easily seen on ultrasound (such as in the pelvis, abdomen, or if an upper extremity clot is extending into the chest), a CT Venogram (or in some cases MRI Venogram) might be utilized. These can also screen for pulmonary embolism if you have chest symptoms. For example, a CT pulmonary angiography can simultaneously look for clots in the lungs and large leg veins.
- Blood tests for clotting disorders: If you have repeated clots or an unusual clot (like in the arms or an abdominal vein) or a strong family history, your doctor may order blood tests to look for inherited clotting tendencies. Identifying a predisposition can guide how long you need treatment and if your family members should be tested.
At Dr. Darryl Lim’s clinic, we emphasize fast and accurate diagnosis. If you come in with signs of a possible DVT, we can perform a duplex ultrasound scan promptly on the same day. Early confirmation allows us to begin treatment immediately, which is essential for preventing clots from growing or breaking off. Our clinic’s ability to both diagnose (with ultrasound) and treat DVT means you receive seamless care under one roof.
Treatment Options for DVT
DVT treatment has two main objectives: stop the clot from traveling to the lungs, and prevent extension of the existing clot. A comprehensive approach often involves medication, lifestyle measures, and in certain cases, procedures to remove or neutralize the clot. The treatment strategy will depend on the severity and location of the clot, as well as the patient’s overall health.
1. Medications (Anticoagulation)
For most DVT patients, the cornerstone of treatment is anticoagulation – often referred to as “blood thinning” medication. These drugs don’t directly dissolve the clot, but they reduce the blood’s tendency to clot, preventing the existing clot from growing larger. This gives time for the body to gradually break down the clot on its own. Commonly used anticoagulant medications include:
· Low Molecular Weight Heparin (LMWH): These are injections (such as enoxaparin) given daily. Often used initially or for shorter-term treatment (for example, in pregnant patients or those who can’t take oral meds).
- Warfarin (Coumadin): An oral anticoagulant that has been used for decades. Warfarin is effective but requires monitoring with blood tests (INR levels) and can be affected by diet and other drugs.
- Direct Oral Anticoagulants (DOACs): Newer oral medications like rivaroxaban, apixaban, or dabigatran. These have the advantage of fixed dosing and no need for regular blood-test monitoring in most cases. They are commonly used now for DVT treatment unless there are contraindications.
Typically, a person with DVT will be on anticoagulation therapy for at least 3 to 6 months. In certain cases – such as those with a genetic clotting disorder, recurrent clots, or an ongoing risk factor – longer treatment, or even lifelong anticoagulation, may be recommended.
2. Compression Stockings & Leg Elevation
Compression stockings and leg elevation don’t dissolve the clot, but they’re important in easing symptoms and preventing long-term complications. Compression stockings gently squeeze the legs to improve circulation, helping reduce swelling and discomfort- possibly by 50% or more when worn regularly.
They also lower the risk of post-thrombotic syndrome, a condition that can cause ongoing leg pain, swelling and ulceration after a DVT. Many patients are advised to wear knee-high stockings for several months to a year, depending on symptoms.
Elevating the leg, especially in the early days, can also help drain pooled blood. Propping the leg up on pillows above heart level when resting is a simple way to ease swelling and support recovery.
3. Lifestyle Measures and Monitoring
We encourage patients to stay active as soon as it’s safe. Regular walking, especially with compression stockings, helps circulation and recovery. If sitting for long periods, take short breaks or do simple foot exercises like ankle circles.
Stay well-hydrated, as dehydration can make blood more prone to clotting. While on blood thinners, be mindful of bruising or bleeding and avoid injuries to the affected leg.
4. Advanced Treatments: Minimally Invasive Procedures
While medication is sufficient for many DVT cases, some patients with extensive clots (such as iliofemoral DVT), or severe symptoms (like phlegmasia cerulea dolens) may benefit from more direct intervention. These procedures can help restore blood flow, reduce long-term vein damage, and lower the risk of post-thrombotic syndrome (PTS).

At Dr. Darryl Lim’s practice, we offer the full range of minimally invasive DVT treatments in Singapore. These minimally invasive procedures are performed in a hospital setting under imaging guidance, but they do not require large incisions. Recovery from catheter-based treatments is generally quicker and easier than open surgery. These treatments include:
While medication is sufficient for many DVT cases, some patients with extensive clots (such as iliofemoral DVT), or severe symptoms (like phlegmasia cerulea dolens) may benefit from more direct intervention. These procedures can help restore blood flow, reduce long-term vein damage, and lower the risk of post-thrombotic syndrome (PTS).
At Dr. Darryl Lim’s practice, we offer the full range of minimally invasive DVT treatments in Singapore. These minimally invasive procedures are performed in a hospital setting under imaging guidance, but they do not require large incisions. Recovery from catheter-based treatments is generally quicker and easier than open surgery. These treatments include:
- Catheter-Directed Thrombolysis: In this procedure, a thin catheter is inserted into the vein (usually via a small puncture in the groin) and guided to the site of the clot under imaging. A “clot-busting” drug (thrombolytic) is delivered directly into the clot through the catheter, helping dissolve it. This method is especially useful for very fresh clots of a few days duration. By breaking up the clot quickly, thrombolysis can restore blood flow.
- Mechanical Thrombectomy: Here, specialized devices are used to physically remove or break up the clot. Devices like the AngioJetTM thrombectomy catheter may work by suction (vacuuming out the clot) or by fragmentation (breaking the clot into smaller pieces) which are then removed. Mechanical thrombectomy is often done in combination with catheter thrombolysis. It’s very effective for large clots, and modern devices allow us to clear clots with just a small catheter puncture, avoiding traditional open surgery in many cases.
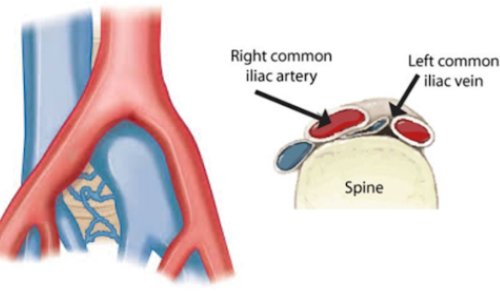
- Angioplasty and Stenting: Sometimes a DVT is associated with an underlying narrowing in a vein (for example, May-Thurner syndrome where the left iliac vein is compressed). In such cases, after clearing the clot, we might perform balloon angioplasty to widen the vein and then place a venous stent (a small metal mesh tube) to keep the vein open. This helps improve long-term blood flow and prevent re-clotting in that area. Venous stenting is typically done for larger calibre veins (like the iliac veins in the abdomen)

Inferior Vena Cava (IVC) Filter: In select cases where a patient cannot take blood thinners (e.g. due to bleeding risk) or when there’s concern about clot migration during a procedure, we may consider placing an IVC filter. This small metal device is implanted in the inferior vena cava — the main vein returning blood from the lower body to the heart — where it acts as a safety net, catching clots before they can travel to the lungs. The filter is inserted via a minimally invasive puncture in the groin or neck.
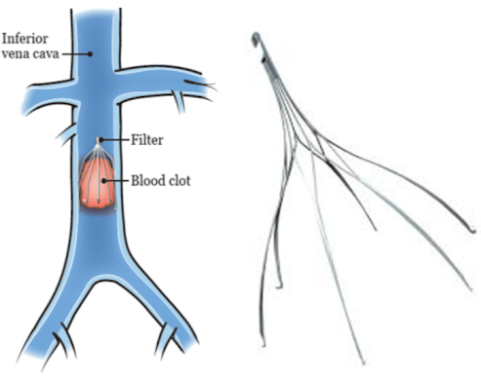
Most modern filters are retrievable and are typically removed a few weeks after thrombolysis or thrombectomy. While IVC filters don’t treat the clot itself, they can be life-saving by preventing pulmonary embolism (PE) in high-risk situations.
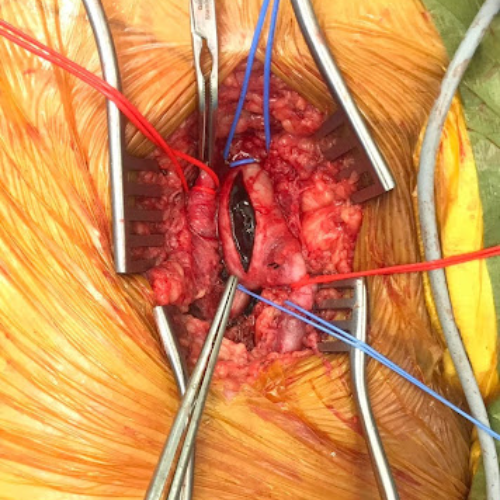
5. Open Surgical Thrombectomy
Open surgery for DVT is now uncommon, since minimally invasive methods have become so effective. An open thrombectomy involves making an incision directly over the vein (typically in the groin) and removing the clot manually. This might be considered if the clot is very large, longstanding, and causing a limb-threatening condition that did not improve with other methods. Open surgery generally involves a longer recovery, so it’s typically not a first line surgical option – but it remains an important option for comprehensive DVT care. Having the capability to perform open surgery means every treatment modality is available to our patients, all under one vascular specialist’s care.

Preventing DVT and Aftercare
Prevention plays a key role in reducing the risk of developing DVT — or having it come back. If you’ve had a DVT before, your doctor will recommend simple lifestyle changes to protect your veins:
• Stay active: Daily walking or light exercise keeps blood flowing. Avoid sitting for long periods without moving.
• Maintain a healthy weight: Reducing excess weight eases pressure on your leg veins.
• Avoid smoking: Quitting smoking improves circulation and lowers your risk of clotting.
• Use compression when advised: Especially during travel, after surgery, or if you’ve had a previous DVT.
• Stay well-hydrated: Drink water regularly — especially in hot weather — and go easy on alcohol.
Ongoing follow-up is important. We may recommend periodic ultrasounds to monitor clot resolution and watch for signs of post-thrombotic syndrome, a condition marked by chronic swelling and discomfort. Early detection allows us to intervene with measures like compression therapy or targeted treatments. We tailor your care based on progress, ensuring the safest and most effective recovery plan.
Your Trusted Partner for DVT Treatment in Singapore
Facing Deep Venous Thrombosis can be overwhelming — but expert care is close at hand. At Dr. Darryl Lim’s clinic, we offer comprehensive DVT care, from on-site ultrasound diagnosis to a full range of treatments, including medication, minimally invasive procedures, and surgery when needed.
Every patient’s situation is different, and we tailor our approach accordingly. Whether your case is straightforward or complex, early diagnosis and intervention can make all the difference.
If you’re experiencing leg pain, swelling, or have concerns about your DVT risk, don’t wait. Reach out for a consultation — with the right care, most DVTs are highly treatable, and you can take meaningful steps to protect your vascular health.










